Immunosuppressants: What They Are, How They Work, and What You Need to Know
When your immune system goes too far—attacking your own body or rejecting a new organ—immunosuppressants, drugs that reduce the activity of the immune system to prevent damage. Also known as anti-rejection meds, they’re not just for transplant patients. These drugs help people with lupus, rheumatoid arthritis, Crohn’s disease, and other autoimmune conditions live without constant inflammation and pain. Without them, many wouldn’t survive a transplant. With them, some manage chronic illness for decades. But they’re not harmless. Taking an immunosuppressant means your body can’t fight off infections the way it used to. That’s why tracking side effects, avoiding live vaccines, and watching for signs of illness are just as important as taking the pill on time.
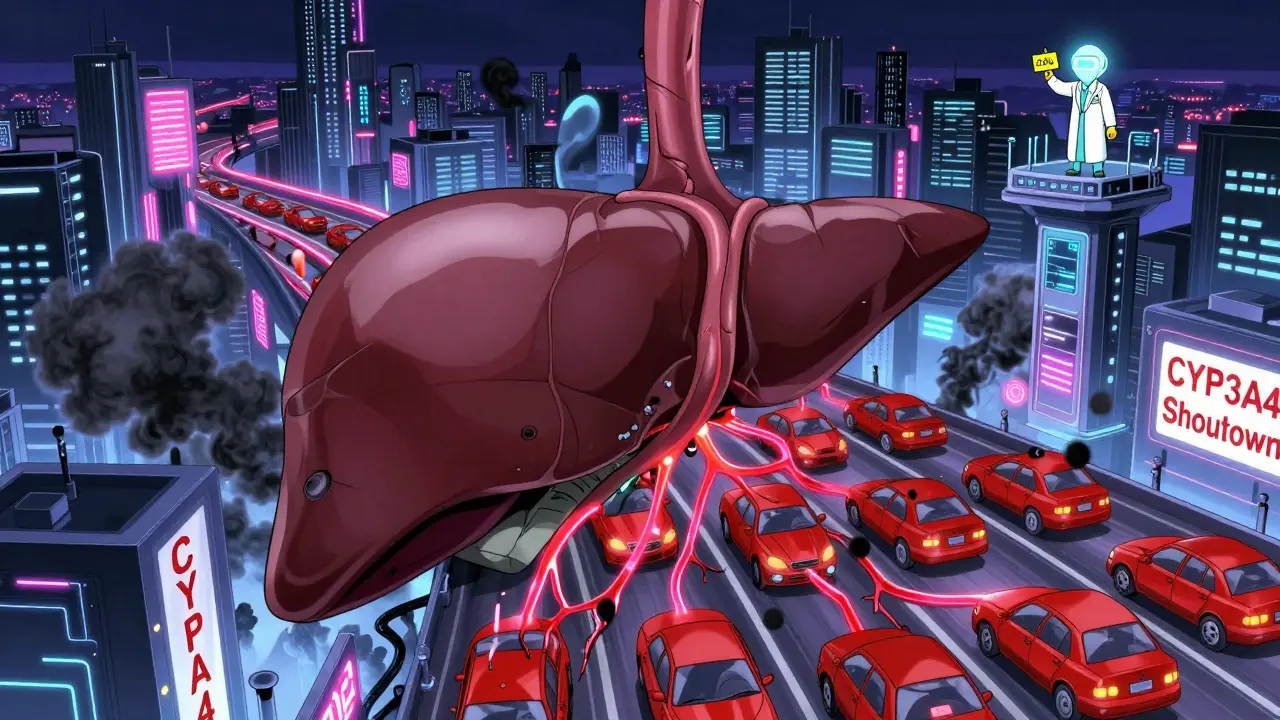
These drugs don’t all work the same way. cyclosporine, a calcineurin inhibitor that blocks T-cell activation was one of the first breakthroughs in transplant medicine. Today, tacrolimus, a similar but more potent drug often used after liver or kidney transplants has largely replaced it in many cases. Then there are drugs like azathioprine and mycophenolate, which slow down the production of immune cells. Steroids like prednisone are used short-term to kickstart control but avoided long-term because of bone loss, weight gain, and diabetes risks. Each drug has its own profile—what it protects, what it harms, and what it interacts with. Some, like sirolimus, even help prevent cancer growth in transplant patients, while others increase the risk. Knowing which one you’re on—and why—makes all the difference.
What you won’t find in most drug labels is how these meds affect daily life. You might need to skip the farmer’s market because of moldy fruit. You might avoid crowded places during flu season. You might need to adjust your dose if you get a fever. And you’ll definitely need regular blood tests to check kidney function and drug levels. Many patients on these drugs also take other meds for blood pressure, cholesterol, or acid reflux—some of which can dangerously interact. That’s why communication with your pharmacist and doctor matters more than ever. It’s not just about taking pills. It’s about managing a delicate balance between staying alive and staying well.
The posts below cover real situations where immunosuppressants come into play—from transplant care to managing autoimmune flare-ups. You’ll find advice on avoiding dangerous drug interactions, how to handle side effects without quitting treatment, and what to ask your doctor when things feel off. These aren’t theoretical guides. They’re written by people who’ve lived it—and they’ll help you do the same.
Systemic Antifungals and Statins: What You Need to Know About Dangerous Drug Interactions
Systemic antifungals like azoles can dangerously raise statin levels, leading to muscle damage or rhabdomyolysis. Learn which combinations are risky, which statins are safer, and how to avoid life-threatening interactions.
Immunosuppressants: Essential Safety Tips for Transplant Patients
Immunosuppressants prevent organ rejection after transplant but carry serious risks like infection, cancer, and kidney damage. Learn how to take them safely, avoid missed doses, and manage long-term side effects for the best outcomes.