When you’re on a statin to lower cholesterol and suddenly need an antifungal for a stubborn yeast infection or fungal pneumonia, things can get dangerous-fast. These aren’t just theoretical risks. Real people end up in the hospital with muscle damage so severe it can kill. The problem? Many doctors and patients don’t realize how common and deadly these interactions are.
Why Azole Antifungals Are a Silent Threat
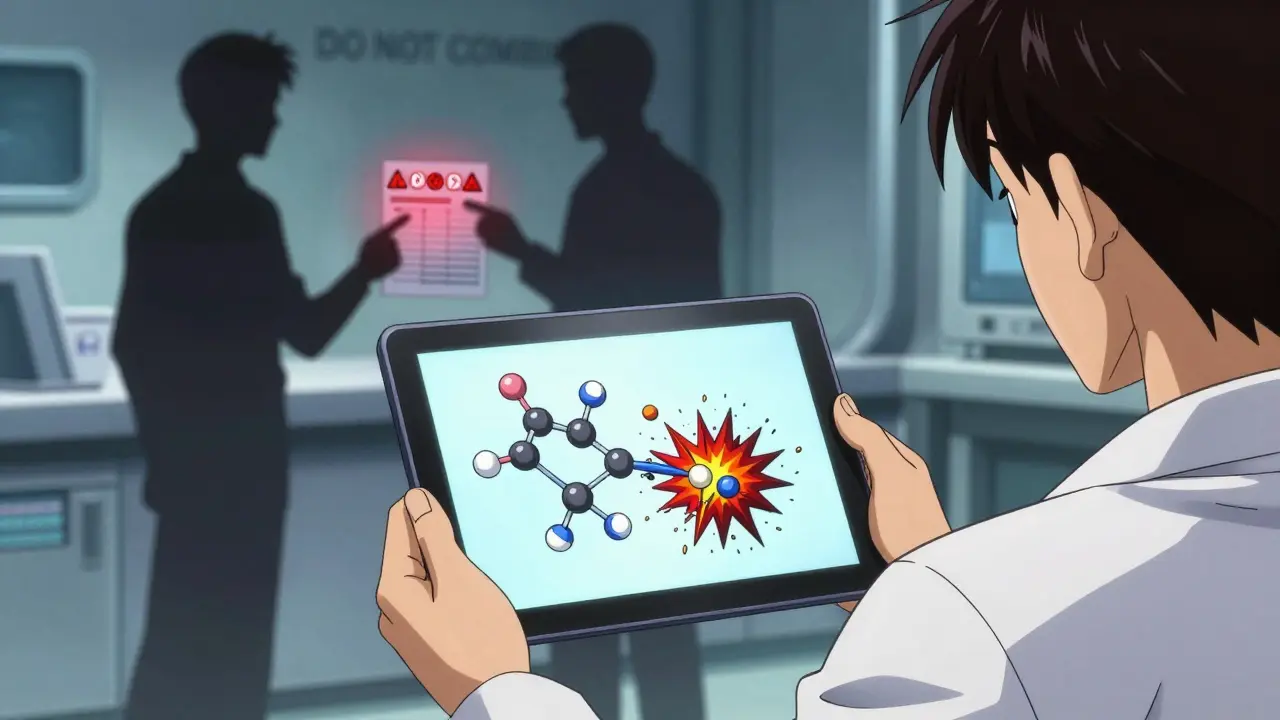
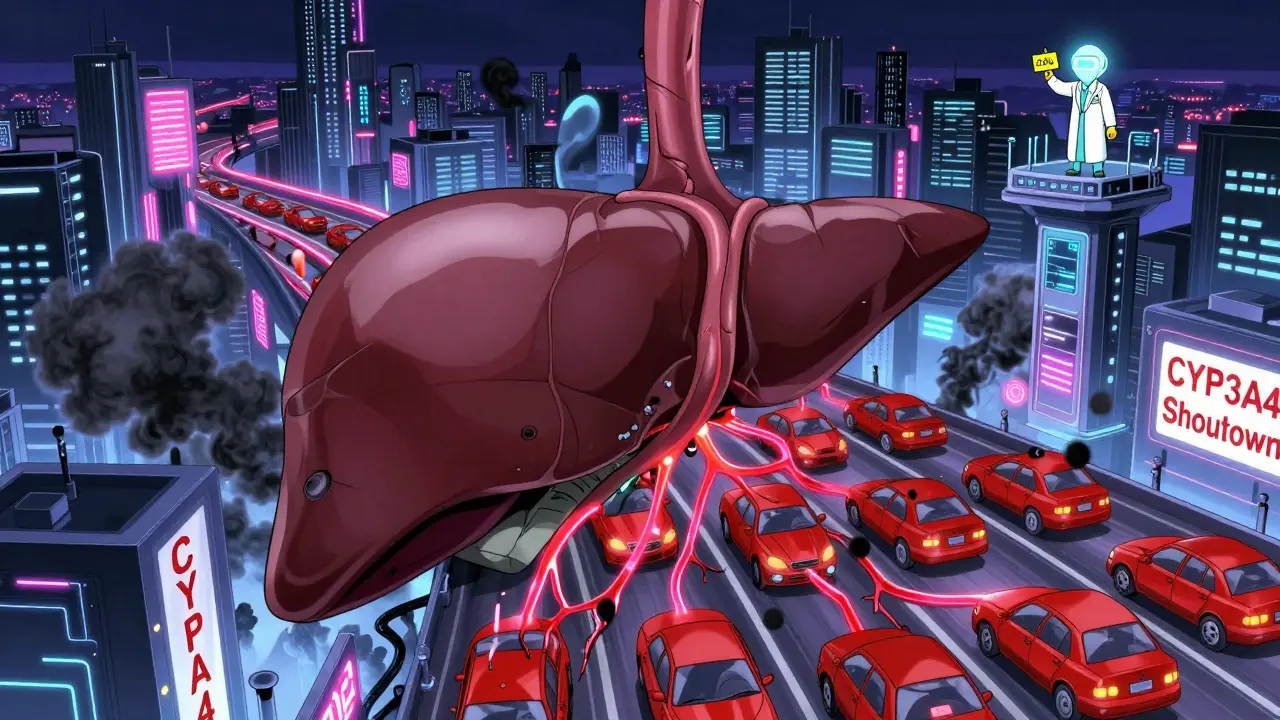
Systemic antifungals like fluconazole, itraconazole, voriconazole, and especially ketoconazole and posaconazole don’t just kill fungi. They also shut down key enzymes in your liver that break down other drugs. These enzymes, especially CYP3A4, handle about 30% of all medications your body processes. When azoles block them, statins and immunosuppressants pile up in your bloodstream like traffic jams.Think of CYP3A4 as a tollbooth. Statins like simvastatin and atorvastatin need to pass through it to get broken down and cleared. Azole antifungals are like roadblocks. They don’t just slow traffic-they stop it completely. That’s why simvastatin levels can spike 15 to 20 times higher than normal when taken with itraconazole. That’s not a side effect. That’s a chemical overload.
Statins That Are Most at Risk
Not all statins are created equal. Some are far more vulnerable to these interactions.- High risk: Simvastatin, lovastatin, atorvastatin - all heavily processed by CYP3A4. These are the ones most likely to cause muscle damage.
- Lower risk: Pravastatin and rosuvastatin - they don’t rely much on CYP3A4. That’s why they’re often the go-to when you need an antifungal.
But here’s the catch: even pravastatin and rosuvastatin aren’t safe with ketoconazole. Why? Because ketoconazole doesn’t just block CYP3A4. It also shuts down OATP1B1, a transporter that pulls statins out of your blood and into your liver for processing. Block that, and even the "safer" statins start building up.
Immunosuppressants Make It Worse
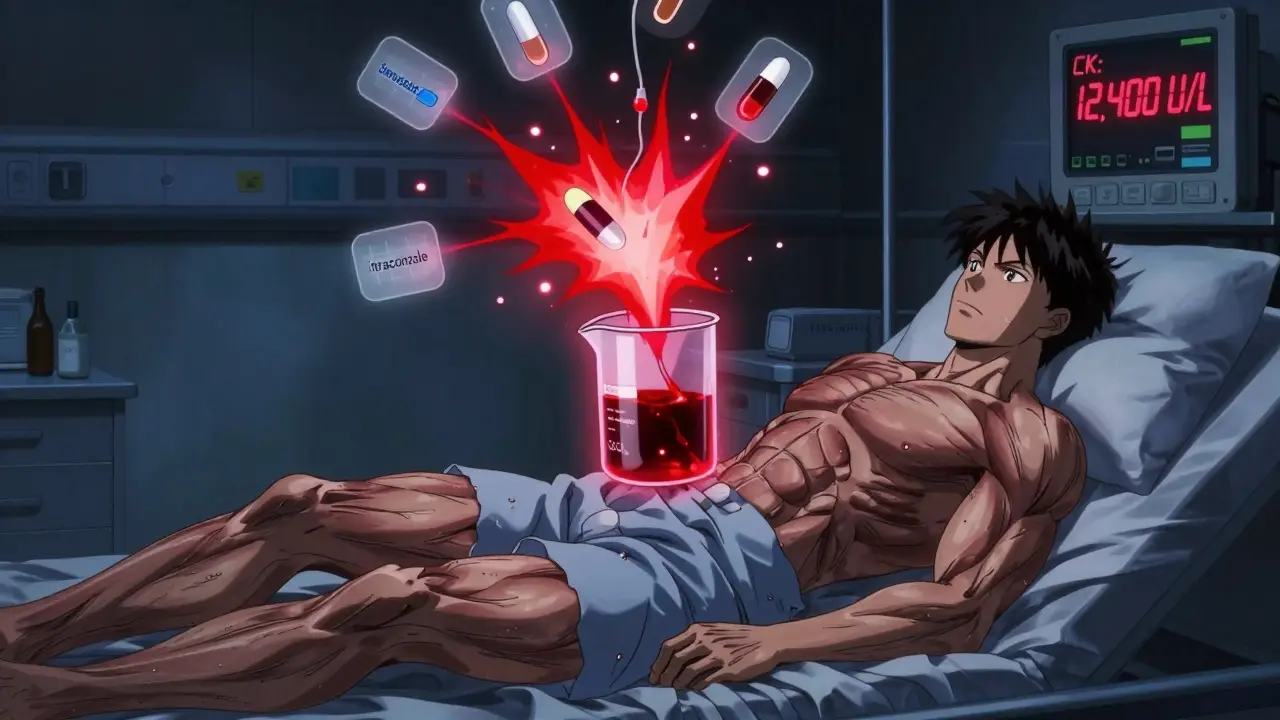
If you’ve had a kidney, liver, or heart transplant, you’re likely on cyclosporine, tacrolimus, or sirolimus. These drugs keep your immune system from rejecting the new organ-but they also inhibit CYP3A4 and P-glycoprotein. That means they do the same thing as azole antifungals: they trap statins in your blood.Studies show that in transplant patients, combining statins with cyclosporine can boost statin levels by 3 to 20 times. That’s why muscle pain and weakness aren’t just "annoying side effects" here-they’re warning signs of rhabdomyolysis. In extreme cases, creatine kinase (CK) levels have soared past 10,000 U/L. Normal is under 200. When CK hits 10 times that, your muscles are literally breaking down. That can lead to kidney failure. And death.
What Happens When Statins Go Too High
Statin-related muscle damage doesn’t always start with pain. Sometimes, it starts with fatigue. Or dark urine. Or just feeling off. But when levels get dangerously high, the body starts breaking down muscle tissue. That’s myopathy. When it gets worse, it’s rhabdomyolysis.Here’s what that looks like in real life:
- Severe muscle soreness, especially in thighs and shoulders
- Weakness so bad you can’t climb stairs or lift your arms
- Urine that looks like cola or tea
- Swelling in limbs
These aren’t rare. A 2012 study found that statin-azole combinations were prescribed more often than they should be-even though labels warned against it. People get sick because the risks aren’t always flagged in busy clinics. A pharmacist catches it. A nurse questions it. But too often, it slips through.
How to Stay Safe
If you’re on a statin and need an antifungal, here’s what actually works:- Stop high-risk statins. If you’re on simvastatin, lovastatin, or atorvastatin, pause them during antifungal treatment. Don’t just reduce the dose-stop completely.
- Switch to pravastatin or rosuvastatin. These are your safest options. Even then, use the lowest effective dose-10 mg of pravastatin or 5-10 mg of rosuvastatin daily.
- Never combine ketoconazole with any statin. It’s banned for this reason in many countries. If your doctor suggests it, ask for an alternative.
- Watch for posaconazole. It sticks around in your body for over a day. Even after you stop it, your statin shouldn’t restart for at least 2-3 days. And monitor CK levels before restarting.
- Test your CK. If you’re on immunosuppressants and statins, get your creatine kinase checked every 2-4 weeks. If it’s over 10 times the normal limit, stop the statin immediately.
What About Newer Antifungals?
Good news: the landscape is changing. Isavuconazole, approved in 2015, is a moderate CYP3A4 inhibitor-not as bad as ketoconazole. And olorofim, currently in trials, doesn’t touch CYP enzymes at all. It kills fungi in a completely different way. If approved, it could be a game-changer for people on statins or transplant meds.Pharmacists are also stepping up. In 87% of major U.S. hospitals, a pharmacist now reviews every antifungal prescription before it’s dispensed if the patient is on a statin. That’s cut dangerous combinations by 63%. But outside academic centers? Many community pharmacies still don’t have those safeguards.
What You Should Ask Your Doctor
Don’t wait for them to bring it up. Ask these questions:- "Is this antifungal going to interfere with my statin?"
- "Can we switch me to pravastatin or rosuvastatin during this treatment?"
- "Do I need to stop my statin completely? If so, for how long?"
- "Should I get a blood test for creatine kinase before and after?"
If your doctor says, "It’s fine," push back. Show them the data. Ask if they’ve seen cases of rhabdomyolysis from this combo. Most haven’t. But that doesn’t mean it doesn’t happen.
The Bottom Line
This isn’t about avoiding treatment. It’s about avoiding preventable harm. Fungal infections need to be treated. Cholesterol needs to be managed. But doing both at the same time without planning is like driving with your brakes and gas pedal pressed down.The safest path? Work with your pharmacist. Ask your doctor to check interaction databases like the University of Liverpool’s Antifungal Interaction Checker. And if you feel unexplained muscle pain, weakness, or dark urine-stop the statin and get help. Your muscles, and your kidneys, will thank you.
Can I take fluconazole with my statin?
Fluconazole is a moderate CYP3A4 inhibitor and a strong CYP2C19 inhibitor. It’s safer than ketoconazole or posaconazole, but still risky with simvastatin, lovastatin, or atorvastatin. If you’re on one of those, switch to pravastatin or rosuvastatin. Even then, use the lowest dose and monitor for muscle pain. Fluconazole is usually okay with pravastatin or rosuvastatin at standard doses, but never assume it’s safe without checking.
What if I’m on cyclosporine after a transplant?
Cyclosporine dramatically increases statin levels-by up to 20 times. Statins like simvastatin and atorvastatin are dangerous here. Pravastatin or rosuvastatin at low doses (10 mg or less) are the only options. You’ll need regular blood tests for creatine kinase and kidney function. Never start or increase a statin dose without your transplant team’s approval.
Is it safe to restart my statin after finishing an antifungal?
Not right away. Azoles like posaconazole stick around in your body for 24-30 hours, and their effects on enzymes last even longer. Wait at least 3-5 days after your last dose before restarting a statin. If you were on a high-risk statin like simvastatin, restart with a low dose and check CK levels first. If you feel muscle pain after restarting, stop immediately and call your doctor.
Why don’t doctors know about this more often?
Many don’t. Statins and antifungals are both common. Doctors focus on treating the infection or lowering cholesterol-not the hidden interaction. Electronic systems help, but not all clinics use them. A 2012 study found these dangerous combos were still prescribed regularly despite clear warnings. The burden often falls on patients to ask the right questions.
Are there any statins that are completely safe with antifungals?
No statin is 100% safe with all antifungals. But pravastatin and rosuvastatin are the safest options because they’re not primarily broken down by CYP3A4. Even so, ketoconazole can still raise their levels by blocking OATP1B1. The key is using the lowest effective dose, avoiding ketoconazole entirely, and monitoring for symptoms. Always check with your pharmacist before combining any antifungal with any statin.
Sarah Triphahn
My cousin ended up in the ER last year after taking fluconazole with simvastatin. He thought he was fine because he didn’t have pain-just felt ‘weirdly tired.’ Turns out his CK was 12,000. They didn’t even warn him. This post? It’s the reason I now print out drug interaction charts and hand them to my doctors. No more assumptions.
Stop being passive. Read the damn label. Or better yet, talk to your pharmacist before swallowing anything.
Vicky Zhang
Oh my god, I’m crying right now. I just got off the phone with my cardiologist and realized I’ve been on atorvastatin for three years while getting monthly fluconazole for recurrent yeast infections. I thought the ‘muscle soreness’ was just from yoga. I’m switching to pravastatin tomorrow. I’m so scared but also so grateful someone finally spelled this out like I’m not a medical student.
You’re not just saving my muscles-you’re saving my life. Thank you. From the bottom of my heart. I’m sharing this with every woman I know who’s ever been told ‘it’s just a yeast thing.’ It’s not just a yeast thing. It’s a death sentence waiting to happen.
I’m printing this. Framing it. Putting it on my fridge.
Sarah -Jane Vincent
Oh please. This is Big Pharma fearmongering. You think they really care if you get rhabdomyolysis? Nah. They make more money off your kidney failure and dialysis. Fluconazole? It’s just a fungus killer. Statins? They’re just cholesterol blockers. Why would they interact? Because the FDA lets them. Because the AMA is paid off. Because your doctor’s too busy watching TikTok to read the manual.
I’ve been on ketoconazole and simvastatin together for five years. No issues. My CK is normal. My muscles are strong. Your ‘danger’ is just a marketing ploy to sell you ‘safer’ statins that cost three times more. Wake up.
Also, posaconazole? That’s just a fancy name for a drug that’s been banned in Europe. Coincidence? I think not.
Henry Sy
Man, I had a buddy who got rhabdo from this combo. Dude was 42, lifted weights, ate clean-thought he was invincible. Then he took itraconazole for a toenail fungus and woke up one morning unable to stand. His legs were swollen like balloons. They had to dialyze him for two weeks.
He still takes statins now, but only rosuvastatin 5mg. And he swears by his pharmacist. Says that guy’s the real MVP. Honestly? I stopped trusting doctors after this. My pharmacist knows more about my meds than my cardiologist does. He’s got a spreadsheet on me. I’m not even joking.
Also, if your doctor says ‘it’s fine,’ ask them if they’ve ever seen someone die from this. If they say no? Walk out.
Anna Hunger
While the general sentiment expressed herein is clinically accurate and aligns with current guidelines from the American College of Cardiology and the European Society of Cardiology, it is imperative to emphasize that the risk stratification for statin-azole interactions must be individualized based on pharmacokinetic profiles, renal function, concomitant medications, and genetic polymorphisms such as SLCO1B1 variants.
Pravastatin and rosuvastatin are indeed preferable, but even these agents may exhibit altered bioavailability in patients with hepatic impairment or those concurrently using potent OATP1B1 inhibitors such as cyclosporine. Therefore, therapeutic drug monitoring and creatine kinase surveillance remain non-negotiable components of safe prescribing.
Further, the assertion that ketoconazole is universally contraindicated is correct; however, its use in rare, life-threatening fungal infections under strict pharmacovigilance protocols may still occur in specialized centers. Such exceptions do not invalidate the broader safety principle.
Patients are encouraged to maintain a current, annotated medication list and to consult with a clinical pharmacist prior to initiation of any new systemic antifungal agent.
Jason Yan
This whole thing hits me like a punch to the gut-not because I’m scared, but because it’s so stupidly preventable.
We live in a world where we can send rockets to Mars but can’t get a simple alert in our EHR when someone’s on simvastatin and fluconazole. Why? Because the system isn’t built to protect people-it’s built to move patients through. Doctors are drowning in paperwork. Pharmacists are understaffed. Patients? They’re told to ‘take this’ and ‘come back in three months.’
And yet, the solution is so simple: ask. Check. Switch. Monitor.
It’s not about being paranoid. It’s about being awake. We’ve been trained to trust the white coat, but the white coat doesn’t always know. The real wisdom? It’s in the pharmacy counter, the nurse who catches the error, the patient who reads the leaflet.
So yeah-ask your doctor. Ask your pharmacist. And if they roll their eyes? Find someone who doesn’t.
Because your muscles aren’t replaceable. And neither is your life.
shiv singh
You people are so weak. My uncle took ketoconazole and Lipitor for years. He didn’t die. He got stronger. You’re all scared of your own shadows. Why don’t you just take your statins and shut up? The real problem is that you’re all too lazy to read the label. Or maybe you’re just addicted to being scared of everything.
Also, why are women always crying about their muscles? Men don’t whine. We just take it. You think your body’s fragile? It’s not. It’s your mind that’s broken.
Stop listening to these ‘experts.’ Go lift weights. Drink water. Stop being a victim.
Robert Way
hey so i just got prescribed fluconazole and i take atorvastatin and i read this and now i dont know what to do. i dont even know what cyp3a4 is. can someone just tell me if i should stop my statin? i dont wanna end up in the er but i dont wanna get a yeast infection either. help plz. also can i just take a lower dose of both? like half a pill? thanks lol