Demodex Ivermectin: Effective Treatments and Practical Guidance
When you explore demodex ivermectin, the therapeutic use of ivermectin to eradicate Demodex mites that cause skin and eye problems. Also known as Ivermectin for Demodex, it bridges parasite control and dermatology, offering a targeted way to lower mite counts and ease related irritation.
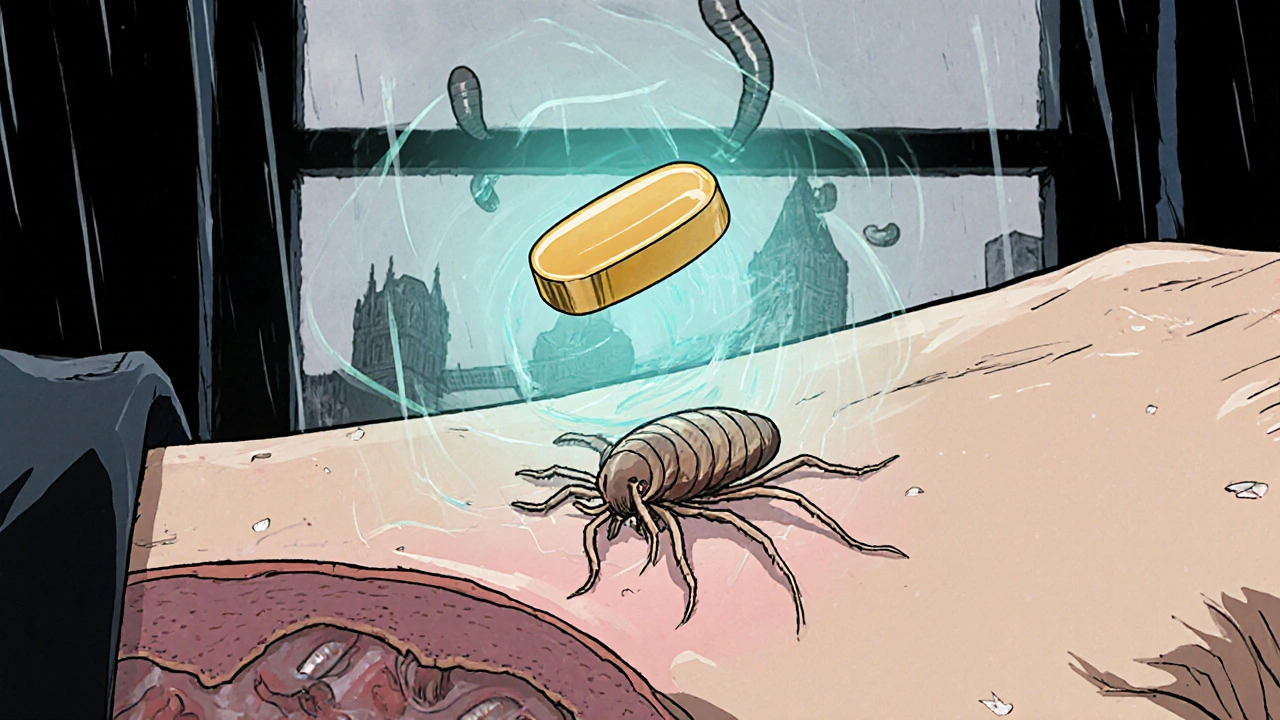
The culprit behind most cases is the Demodex mite, a microscopic parasite that lives in hair follicles and sebaceous glands. When populations explode, patients often notice redness, itching, or the flaky patches common in rosacea. Ivermectin, a broad‑spectrum antiparasitic, interferes with the mite’s nerve signals, leading to paralysis and death. This simple cause‑effect relationship—Demodex ivermectin reduces mite density—forms the backbone of most treatment plans. The drug can be applied topically as a 1% cream or taken orally in low‑dose regimens, depending on the severity and location of the infestation.
Key Considerations for Using Ivermectin Against Demodex
Understanding where Demodex shows up helps pick the right approach. On the face, especially around the nose and cheeks, the mite contributes to rosacea, a chronic inflammatory skin condition. Studies show that clearing the mites often leads to clearer skin and fewer flare‑ups—a clear example of rosacea severity improves after Demodex eradication. Around the eyes, the same organisms can trigger blepharitis, causing crusty eyelid margins and discomfort. In such cases, a short course of oral ivermectin combined with lid hygiene tends to work faster than creams alone because the drug reaches deeper follicular zones.
Dosage matters. For topical use, applying a pea‑sized amount once daily for 2–4 weeks usually suffices; many clinicians then taper to every other day to maintain control. Oral dosing often starts at 200 µg/kg on day 1, followed by a repeat dose one week later; this protocol mirrors how ivermectin treats other parasitic infections while keeping systemic exposure low. Proper dosing requires monitoring for toxicity, especially in patients with liver or kidney impairment. Side effects are generally mild—possible itching or a transient burning sensation at the application site, and rare cases of nausea with oral pills.
Interaction awareness is essential. Ivermectin shares metabolic pathways with several common drugs, such as certain anticonvulsants and cholesterol‑lowering agents. A quick review of a patient’s medication list can prevent unexpected increases in ivermectin levels, which could raise the risk of neurotoxic symptoms. For those who can’t tolerate ivermectin, alternatives like albendazole or mebendazole exist, but they often lack the same skin‑penetration profile and may need longer treatment courses.
Beyond the medication itself, lifestyle tweaks boost results. Maintaining a clean facial routine, avoiding heavy oils, and using a gentle exfoliant keep follicles open for the drug to work. A diet rich in omega‑3 fatty acids can also calm inflammation, supporting the skin’s healing environment. When patients combine these habits with a well‑planned ivermectin regimen, the odds of lasting mite control rise dramatically.
Now that you’ve got the basics of how demodex ivermectin works, its dosing, safety points, and the conditions it influences, the articles below dive deeper into specific scenarios, compare oral versus topical strategies, and explore real‑world outcomes. Keep reading to discover practical tips, patient stories, and expert recommendations that will help you choose the right approach for your situation.
Ivermectin for Skin Parasites: How to Treat Scabies, Larva Migrans & More
Learn how ivermectin treats skin parasites like scabies, larva migrans, demodex and myiasis, with dosing, safety tips, and a comparison table for scabies treatment.