When your blood calcium stays too high for too long, your body starts breaking down. Not from eating too much dairy or taking too many supplements - but because one of your tiny glands in the neck is sending the wrong signals. That’s hyperparathyroidism. It’s not rare. Around 100,000 Americans are diagnosed each year, and many more go undetected for years because the symptoms are vague: fatigue, joint pain, kidney stones, brain fog. By the time it’s caught, bones may already be thinning, kidneys strained, and nerves affected. The good news? There’s a cure - and it’s surgery.
What’s Really Going On Inside Your Body?
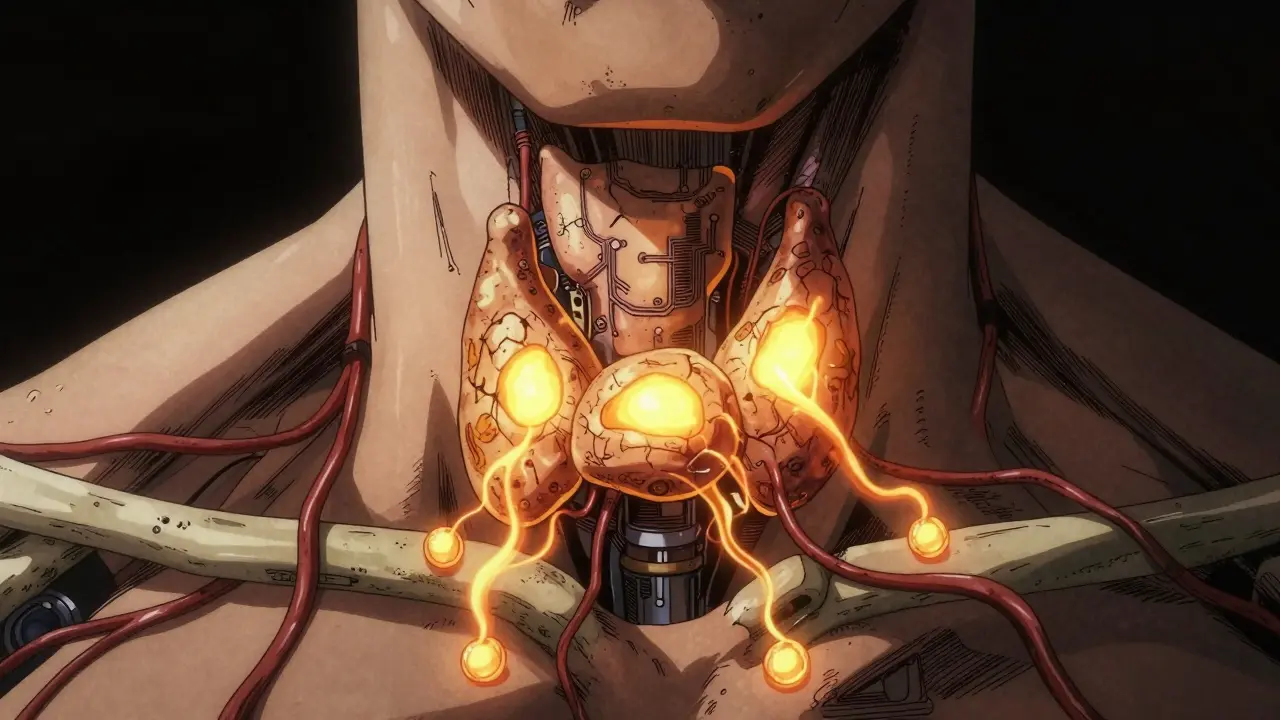
Your four parathyroid glands are no bigger than a grain of rice. They sit behind your thyroid, and their only job is to keep calcium in your blood at the right level. Too low? They release more parathyroid hormone (PTH). Too high? They shut off. Simple, right? In hyperparathyroidism, that switch breaks. One or more glands start pumping out PTH nonstop - even when calcium is already sky-high. This isn’t a mistake. It’s a malfunction. And it triggers a chain reaction:- Stronger signals to your bones: They start dissolving to release calcium into your blood.
- Your kidneys hold onto more calcium instead of flushing it out.
- Your gut absorbs more calcium from food, even if you’re not eating extra.
Why Bone Loss Happens - And Why It’s Dangerous
Your bones aren’t just scaffolding. They’re living tissue, constantly being rebuilt. But when PTH is in overdrive, your body’s bone-builders (osteoblasts) get overwhelmed by bone-breakers (osteoclasts). The outcome? You lose 2 to 4% of bone density every year - mostly in your spine and hips. That might sound small. But over five years, that’s 10 to 20% gone. And that’s not just numbers on a scan. It means fractures become likely. People with untreated hyperparathyroidism are 30 to 50% more likely to break a bone than others their age. A simple fall, a stumble on the stairs - it can end in a hip fracture, surgery, months of rehab. DXA scans show this clearly. In one study, patients with high PTH had spine bone density scores that dropped faster than women going through menopause. And here’s the kicker: even after surgery, if the bone loss was severe, full recovery isn’t guaranteed. Some people need ongoing treatment with bisphosphonates just to stop further damage.Surgery Isn’t Just an Option - It’s the Only Cure
There’s no pill that fixes this. Medications like cinacalcet can lower PTH a bit, but they don’t stop the gland from overproducing. They just manage symptoms. For primary hyperparathyroidism - the most common type - surgery is the only way to cure it. The procedure is called a parathyroidectomy. In 85% of cases, it’s just one bad gland - a benign tumor called an adenoma. Surgeons remove it through a small incision, often under local anesthesia. The operation takes about 90 minutes. Most people go home the same day. Success rates? 95 to 98% when done by experienced surgeons. That’s higher than many common surgeries. And the results aren’t just lab numbers. Patients report:- Energy returning within weeks
- Brain fog lifting - no more forgetting names or losing focus at work
- Kidney stones stopping
- Bone pain fading

Who Needs Surgery - And Who Can Wait?
Not everyone with high calcium needs to rush into the operating room. But the guidelines are clear: if you meet any of these, surgery is recommended:- Your calcium is more than 1 mg/dL above normal
- Your kidney function is dropping (creatinine clearance under 60)
- Your bone density T-score is -2.5 or lower (that’s osteoporosis)
- You’re under 50 years old
What Happens After Surgery?
The biggest surprise for many patients? Their calcium drops too low after surgery. That’s not a complication - it’s expected. When the bad gland is gone, your body needs time to reset. For 30 to 40% of people, calcium dips below normal for a few weeks. You’ll need calcium supplements - often 500 to 1,000 mg three times a day - and sometimes vitamin D. Most people feel fine within a week. But recovery isn’t just about calcium levels. It’s about rebuilding:- Bone density starts to climb 6 to 12 months after surgery - up to 5% in the spine.
- Some patients need to keep taking bone-strengthening meds if damage was severe.
- Annual calcium checks are needed for life, especially if you had multiple bad glands.
Why So Many People Are Diagnosed Late
This condition flies under the radar. Symptoms look like aging, stress, or depression. Fatigue? “You’re just tired.” Joint pain? “You’re getting older.” Kidney stones? “Drink more water.” A 2023 survey found nearly half of patients saw three or more doctors before getting the right diagnosis. Some waited five years. By then, damage was done. The problem? Calcium is often checked during routine blood work - but no one connects the dots. If your calcium is high, PTH should be tested immediately. Too often, it’s not. And if PTH is normal or “in the high-normal range,” doctors assume it’s fine. But in 20% of cases, PTH is inappropriately normal - meaning it should be low, but isn’t. That’s still hyperparathyroidism.
What’s New in Diagnosis and Treatment
Technology is catching up. Five years ago, finding the bad gland meant a long scan and sometimes exploratory surgery. Now:- Technetium-99m sestamibi scans detect adenomas with 90% accuracy.
- 4D-CT scans give 95% accuracy in complex cases.
- AI tools are now helping radiologists spot gland abnormalities faster and with fewer errors.
What to Do If You Suspect You Have It
If you’ve had unexplained fatigue, kidney stones, bone pain, or brain fog - and your calcium was ever high - ask for a PTH test. Don’t wait. Don’t assume it’s nothing. Start with your doctor. Request:- Serum calcium (fasting)
- Parathyroid hormone (PTH)
- 25-hydroxyvitamin D
- Renal function (creatinine, eGFR)
Final Thought: This Isn’t Just a Hormone Problem - It’s a Whole-Body Issue
Hyperparathyroidism doesn’t just affect your bones or your kidneys. It steals your energy, your focus, your quality of life. Left untreated, it’s a slow-motion crisis. But caught early, and treated with surgery, it’s one of the most curable endocrine conditions out there. You don’t need to live with brain fog because your glands are broken. You don’t need to fear a hip fracture because your bones are thinning. The fix exists. It’s safe. It works. And it’s waiting for you to ask the right question: “Could this be hyperparathyroidism?”Can hyperparathyroidism be cured without surgery?
No. Medications like cinacalcet or bisphosphonates can help manage symptoms or slow bone loss, but they don’t fix the overactive gland. Only surgery - removing the faulty parathyroid tissue - can cure primary hyperparathyroidism. That’s why it’s the standard of care for eligible patients.
Is hyperparathyroidism dangerous if I don’t have symptoms?
Yes. Many people feel fine for years, but their bones are still losing density, their kidneys are working harder, and their risk of fractures or kidney stones is rising. Studies show asymptomatic patients have 2 to 3 times higher fracture risk than those with normal calcium. Waiting doesn’t make it safer - it makes recovery harder.
What happens to my calcium levels after surgery?
It’s common for calcium to drop too low right after surgery - this is called transient hypocalcemia. Your body is adjusting to not having excess PTH. Most people need calcium supplements for 2 to 8 weeks. In rare cases, it lasts longer. Your doctor will check your levels at 4, 24, and 72 hours after surgery to guide treatment.
Can hyperparathyroidism come back after surgery?
Yes, but it’s rare. If only one gland was removed (most common case), recurrence is about 2 to 3% over 10 years. If multiple glands were affected and only part was removed, the risk rises to 5 to 10%. Lifelong annual calcium checks are recommended for everyone after surgery, especially if you had multigland disease.
Does surgery affect my voice or cause scarring?
Voice changes are extremely rare with experienced surgeons - less than 1% risk. The nerves controlling your voice run close to the parathyroid glands, but modern techniques and intraoperative monitoring protect them. Scarring is usually a thin, faint line that fades over time. Minimally invasive surgery uses small incisions, often less than an inch.
How long does recovery take after parathyroid surgery?
Most people go home the same day. Pain is usually mild and controlled with over-the-counter meds. You can return to light activities within 2 to 3 days. Full recovery - including energy levels and brain clarity - often takes 2 to 6 weeks. Bone density improvements take months to show up on scans, but many patients feel better within days.
Can I prevent hyperparathyroidism?
No. It’s not caused by diet, lifestyle, or supplements. Most cases are due to a benign tumor (adenoma) or gland enlargement (hyperplasia) with no known trigger. However, you can prevent complications by getting tested if you have symptoms or risk factors. Early diagnosis means early cure - and less damage to your bones and kidneys.
Spencer Garcia
Just had my parathyroidectomy last month. Calcium dropped to 7.8 the next day-scary as hell, but the supplements fixed it. Energy came back in 10 days. Brain fog? Gone. No more forgetting where I put my keys. This isn’t a ‘maybe’-it’s a wake-up call if your calcium’s high.
Delilah Rose
I’ve been living with this for 8 years. Diagnosed after I broke my wrist falling off a curb. My doctor said ‘it’s just aging’-until my PTH was 180 and my spine density was -3.1. Surgery wasn’t glamorous, but it was life-changing. I didn’t realize how much brain fog was normal for me until it vanished. Now I remember names, finish books, and actually sleep through the night. If you’re tired, foggy, or getting kidney stones-get tested. Don’t wait for a fracture to wake you up.
Paula Villete
So… we’re supposed to believe that a tiny gland can steal your entire life and the only fix is a scalpel? And yet, no one knows why it happens. No environmental triggers. No dietary causes. Just… bad luck? I mean, if it’s not preventable and it’s this common, why isn’t every routine blood panel paired with a PTH test? It’s not laziness-it’s systemic negligence. They’d test for a rare cancer faster than this.
John Pearce CP
It’s appalling that American medicine waits for bone density to crater before acting. In Germany, they screen for PTH in anyone over 45 with unexplained fatigue. Here? You need to be on the brink of a hip fracture before they care. This isn’t medicine-it’s triage by default. And the fact that insurance often denies the scan unless you’re symptomatic is a moral failure.
Lindsey Kidd
Just had my surgery 3 weeks ago 🥹 I was so tired I napped after brushing my teeth. Now I’m hiking on weekends. My mom cried when I told her I remembered her birthday this year. I didn’t even know I’d forgotten it before. This isn’t just a medical fix-it’s a soul reset. If you’re reading this and wondering if you should get checked? Yes. Just yes.
Aurora Daisy
Of course it’s surgery. Everything in America is a scalpel and a bill. Meanwhile, in the UK, they monitor and manage. We don’t cut first, ask questions later. You know what’s worse than hyperparathyroidism? A $40,000 hospital bill for a procedure that might’ve been avoided with better nutrition and vitamin D. But no-let’s just slice and dice and profit.
Blow Job
My cousin had this. They found it during a routine check-up-no symptoms. Surgery next week. He’s 38. No one even thought to check PTH until his dad had it and told the doc. It’s wild how many people are walking around with this and think they’re just ‘old before their time.’ You’re not old-you’re broken. And it’s fixable.
Sidra Khan
So… surgery fixes it? But then your calcium crashes and you’re on supplements for months? That sounds like trading one problem for another. And what if you have multiple bad glands? You get cut open again? Sounds like a gamble with your thyroid nerves and your wallet.
Isaac Bonillo Alcaina
People think this is just ‘a gland thing.’ It’s not. It’s a systemic collapse. Your bones aren’t just thinning-they’re dissolving. Your kidneys are being poisoned by calcium crystals. Your brain is drowning in metabolic noise. And you’re being told to ‘drink more water’? This isn’t a lifestyle tweak. It’s a medical emergency disguised as fatigue.
Bret Freeman
They told me I had depression for five years. I lost my job because I couldn’t focus. My wife left me because I was ‘emotionally absent.’ I cried in the doctor’s office when they said it was my parathyroid. Not my mind. Not my laziness. A tiny gland that forgot how to turn off. I’m not healed-I’m reborn. And I’m mad they didn’t test me sooner.
Payson Mattes
Did you know the FDA approved a drug called etelcalcetide in 2024? It lowers PTH by 45%. But they won’t let you use it unless you’re ‘ineligible for surgery.’ Why? Because hospitals make more money cutting you open. Big Pharma doesn’t want you cured-they want you on meds for life. This whole system is rigged. Don’t trust your doctor. Get a second opinion. And check your calcium. Always.
Adarsh Dubey
I’m from India and we don’t have this tested often. But my uncle had it-diagnosed after he got kidney stones and collapsed. Surgery worked. Now he’s fine. The point is: it’s not rare. It’s ignored. If you have fatigue and stones, ask for PTH. No shame. Just ask.
Jillian Angus
My calcium was 10.8 for 3 years. No symptoms. Doctor said ‘it’s fine.’ Then I got a fracture. Turns out my bones were 18% thinner than average. Now I’m 4 months post-op. Still taking calcium. Still scared it’ll come back. But I can walk without pain. That’s worth the scar.
Diana Alime
so i just found out my pth was high and my calcium was 11.2 and i thought i was just stressed?? like i’ve been forgetting my kid’s school pickup for weeks and my joints ache all the time and i thought it was menopause?? but its my glands??
Christine Détraz
I’m not saying surgery isn’t effective. But I’ve seen people who had it and still struggle-brain fog, muscle cramps, anxiety. Recovery isn’t linear. And if you’re older, your body doesn’t bounce back like it used to. The real issue isn’t the surgery-it’s how little we do to support recovery afterward. No rehab. No nutrition counseling. Just ‘take these pills and come back in six months.’ That’s not care. That’s discharge.