It’s 3:15 p.m. Your neighbor suddenly slurs their words, drops their coffee cup, and can’t raise their right arm. They laugh it off: “It’s gone now. Must’ve been nothing.” They walk away. But if you’ve ever seen someone have a TIA, you know this isn’t nothing. It’s a warning flare - and every minute counts.
What’s the real difference between a TIA and a stroke?
A TIA - or transient ischemic attack - isn’t a “mini-stroke.” That term is misleading, dangerous, and outdated. The American Heart Association stopped using it in 2009. Here’s why: a TIA and a stroke aren’t different in how they start. They both begin with the same sudden symptoms: face drooping, arm weakness, slurred speech, vision loss, dizziness, or a terrible headache. The only difference? One leaves permanent damage. The other doesn’t.But here’s the twist: up to 35% of people who think they had a TIA actually had a minor stroke. Advanced MRI scans show brain tissue damage they didn’t know about. So even if symptoms disappear in 10 minutes, you can’t assume it’s harmless. Modern medicine now defines a TIA by what’s not on the scan - no infarction, no dead brain cells. If there’s damage, it’s a stroke, even if the person feels fine the next day.
How fast do symptoms go away?
Most TIA symptoms fade within an hour. In fact, 56% of cases resolve in 10 to 60 minutes. Only 1 in 10 lasts longer than two hours. That’s why people think they’re fine. They wait. They call their doctor for an appointment next week. That’s a mistake.Stroke symptoms, by contrast, don’t vanish. They might get worse. They might stay the same. But they don’t just disappear. If your arm stays weak after 30 minutes, or your speech doesn’t clear up, that’s a stroke. And time is brain.
The ABCD2 score - your risk in 60 seconds
Emergency rooms use a simple tool called ABCD2 to guess your risk of having a stroke after a TIA. It takes less than a minute. Here’s how it breaks down:- A - Age: 60 or older? That’s 1 point.
- B - Blood pressure: Higher than 140/90? Add 1 point.
- C - Clinical symptoms: Weakness on one side? That’s 2 points. Just speech trouble? That’s 1 point.
- D - Duration: Symptoms lasted 60+ minutes? 2 points. 10 to 59 minutes? 1 point.
- D - Diabetes: Do you have it? Add 1 point.
Add them up. A score of 4 or higher? You’re at high risk. Studies show 8.1% of people with a score of 4 or above have a stroke within two days. That’s not a small chance. That’s urgent.
Why calling 911 is non-negotiable
If you see any of these signs - even if they go away - call 911. Not your cousin. Not your GP. 911.Here’s the hard truth: 31% of people wait more than 24 hours to get checked after a TIA. Why? Because they think it’s over. But the truth is, half of all strokes happen within 48 hours of a TIA. The first two days are the deadliest.
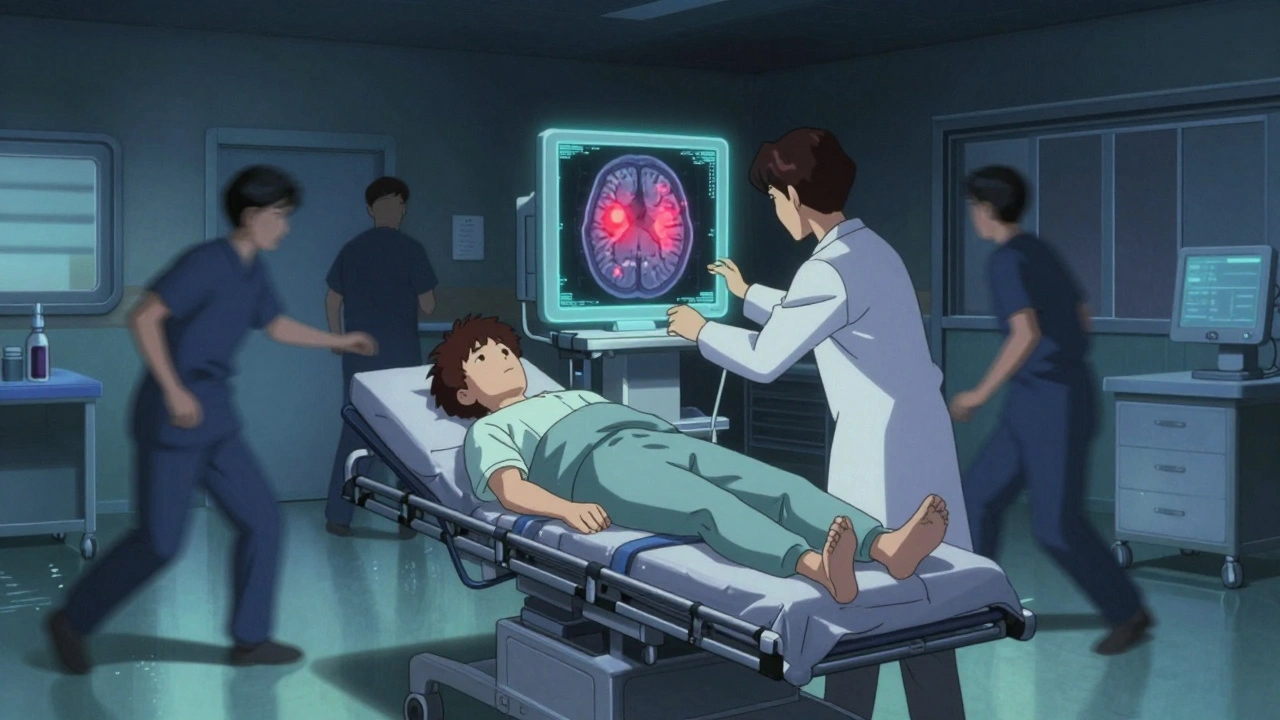
Emergency teams don’t wait. They do a non-contrast CT scan right away to rule out bleeding. Then they get you on an MRI with diffusion-weighted imaging - the only test that can catch tiny areas of brain damage you can’t feel. If the MRI shows injury, it’s not a TIA. It’s a stroke. And you need treatment now.
What happens after the scan?
If it’s confirmed as a TIA, treatment starts immediately - even if you feel fine. The goal isn’t to fix the past. It’s to stop the next one.- Aspirin 325 mg - started within 24 hours - cuts your stroke risk by 60%.
- Dual antiplatelets - aspirin plus clopidogrel - are given for 21 to 30 days for high-risk patients. This combo reduces stroke risk by 80% compared to waiting.
- High-intensity statin - like atorvastatin 80 mg - lowers cholesterol hard and fast. It’s not just about arteries. It’s about stabilizing plaque.
- Blood pressure control - below 140/90 - is mandatory. Many people don’t realize their BP was high until after the TIA.
These aren’t suggestions. They’re standard care. And if you skip them, you’re gambling with your brain.
The myth of “it went away”
The biggest killer here isn’t the TIA itself. It’s the belief that if symptoms vanish, you’re safe. That’s what stops people from acting. That’s what lets strokes happen.Think about this: 1 in 5 people who have a TIA will have a stroke within 90 days. And the biggest risk? The first 48 hours. That’s why programs like SOS-TIA at Massachusetts General Hospital now get 95% of patients evaluated the same day. Their 90-day stroke rate? 1.2%. Without fast action? It’s over 10%.
And here’s something most people don’t know: 48% of TIA patients have hidden brain damage detectable only by advanced MRI. That means even if you feel fine, your brain might already be injured. A TIA isn’t a warning - it’s a sign your brain is already under attack.
What you need to remember: BE FAST
Use this simple tool to spot trouble - whether it’s a TIA or a stroke:- B - Balance: Sudden dizziness, loss of balance or coordination
- E - Eyes: Blurred, double, or lost vision in one or both eyes
- F - Face: One side drooping? Ask them to smile.
- A - Arm: One arm weak? Ask them to raise both.
- S - Speech: Slurred? Strange? Can’t repeat a simple sentence?
- T - Time: Call 911 now. Don’t wait. Don’t drive yourself.
This applies to TIA and stroke. Same signs. Same response. No exceptions.
What’s changing in 2025?
New tools are coming fast. Blood tests for GFAP - a protein released when brain cells are stressed - can now help doctors tell if there’s brain injury in under 15 minutes. Right now, it’s about 48% accurate. By 2026, it’s expected to hit 85%. That means fewer misdiagnoses. Fewer people sent home thinking they’re fine.Hospitals are also using AI to predict stroke risk after TIA with 92% accuracy - far better than the ABCD2 score alone. And insurance rules are changing too. Medicare now penalizes hospitals if more than 20% of TIA patients have a stroke within 30 days. That’s forcing every ER to act fast.
What if you’re the one who had it?
If you’ve had a TIA, you’re not “lucky.” You’re in danger. Your next stroke could be worse. It could be fatal. Or leave you paralyzed, unable to speak, dependent on others.Don’t wait for symptoms to return. Don’t hope it was a fluke. Get the MRI. Take the aspirin. Control your BP. Quit smoking. Manage your diabetes. Start walking. Eat less salt. Take your statin.
These aren’t lifestyle tweaks. They’re survival steps.
Final thought: Your brain doesn’t get a second chance
A TIA is not a rehearsal. It’s the first act of a tragedy you can still stop. Every second you delay, the risk climbs. Every hour you wait, your chance of avoiding a stroke drops.Don’t let the fact that you feel fine fool you. Your brain just had a near-miss. That’s not luck. That’s a signal. And signals like this don’t come twice.
Can a TIA happen without any symptoms?
No. By definition, a TIA causes sudden neurological symptoms - like weakness, speech trouble, or vision loss - that resolve within minutes to hours. If you had no symptoms, it wasn’t a TIA. But silent brain injuries from tiny clots can still happen without obvious signs, which is why MRI scans after a suspected TIA are so important.
Is it safe to wait and see if symptoms come back?
No. Waiting is the most dangerous thing you can do. Up to 5% of people have a stroke within 48 hours of a TIA. That risk drops dramatically if you get treatment within 24 hours. If symptoms go away, you still need emergency care - not a doctor’s appointment next week.
Does a TIA mean I’m going to have a stroke?
Not necessarily - but your risk is very high. About 1 in 5 people who have a TIA will have a stroke within 90 days. That’s why doctors treat it like an emergency. With fast treatment - aspirin, statins, blood pressure control - you can reduce that risk by 80%.
Why is aspirin given right away after a TIA?
Aspirin helps stop blood clots from forming. Starting 325 mg within 24 hours of a TIA cuts your risk of a follow-up stroke by 60%. It’s cheap, fast, and proven. You don’t need to wait for test results - if a TIA is suspected, aspirin is started immediately in the ER.
Can a TIA be seen on a regular CT scan?
Usually not. A standard CT scan can rule out bleeding, but it misses tiny areas of brain damage. That’s why MRI with diffusion-weighted imaging is required. It’s 99% accurate at spotting recent strokes - even ones so small you didn’t feel them.
Are TIAs only a problem for older adults?
No. While the average age is 69, TIAs are happening more often in people under 50 - especially with rising rates of obesity, diabetes, and high blood pressure. Anyone with risk factors - smoking, high cholesterol, atrial fibrillation - should know the signs, no matter their age.
If I feel fine after a TIA, do I still need to see a neurologist?
Yes. Even if you feel 100%, you need a neurologist’s evaluation. They’ll check for hidden causes like carotid artery narrowing, heart rhythm problems, or small vessel disease. Your treatment plan - including medications and lifestyle changes - depends on what they find.
Can stress or anxiety cause TIA-like symptoms?
Anxiety can cause dizziness, tingling, or speech stumbling - but not sudden one-sided weakness, facial drooping, or vision loss in one eye. If you’re unsure, always treat it as a medical emergency. It’s safer to get checked than to assume it’s stress.

Elizabeth Crutchfield
I saw my mom have something like this last year. She laughed it off too. Thought it was just stress. Turned out it was a TIA. We didn’t know until the MRI showed the damage. Don’t wait. Just call 911. 😔
Ben Choy
This is so important. I work in ER and see this every week. People think if it's gone, it's fine. Nope. Half the time they come back 2 days later with a full stroke. Aspirin now. MRI now. No excuses. ❤️
Emmanuel Peter
Let’s be real-most people don’t even know what ABCD2 stands for. And yet they’re Googling symptoms at 2 a.m. and deciding if it’s "worth" calling 911. You’re not a doctor. Your gut isn’t a diagnostic tool. Stop being a dumbass and call the ambulance. Seriously.
Chad Handy
I had a TIA in my 30s. No one believed me. I was too young. My doctor said "it was probably anxiety." Six months later I had a stroke that took my right hand. I’m still rehabbing. The statin saved me. The aspirin saved me. But the delay? That nearly killed me. If you feel even a flicker of weirdness-call 911. Don’t wait for permission. Don’t wait for someone to tell you it’s serious. Your brain doesn’t care how old you are. It just wants you to act.
Augusta Barlow
I think this whole TIA thing is just a way for hospitals to make money. MRI scans cost $2000. Aspirin is 5 cents. Why do they push all this testing? What if it’s just a migraine? Or stress? Or dehydration? I’ve read articles that say 70% of "TIA" cases are misdiagnosed. They scare people into treatments they don’t need. I’m not taking aspirin just because my arm tingled once.
Joe Lam
You people are so dramatic. It’s not a "brain attack." It’s a clot. Big deal. I’ve had worse headaches from beer. The real problem here is medical overreach. You’re turning a minor vascular hiccup into a crisis because insurance wants to bill for MRIs. Wake up.
Chase Brittingham
This post saved my life. My uncle ignored his TIA. Thought he was "just tired." He had a stroke 36 hours later. Lost his speech. Can’t walk. I made sure my whole family knows BE FAST now. If you see it, call 911. No matter how "silly" it feels. Better to be wrong than to lose someone.
Bill Wolfe
Honestly, people who ignore TIA symptoms are just lazy. They don’t want to deal with the truth-that their lifestyle is killing them. Smoking? Check. Fast food? Check. No exercise? Check. You think your body’s gonna let you get away with that? The TIA is your body screaming. You’re choosing to cover your ears. And now you want to blame the doctors? Pathetic.
Michael Feldstein
I’m a paramedic and I’ve seen everything. One time a guy said he felt "weird" and his wife said "it’s probably just indigestion." I told him to get checked. He said no. Two hours later he collapsed. Turned out it was a TIA that became a stroke. He’s fine now-thanks to the ER team. But he almost didn’t make it. Don’t be that guy. Don’t be that wife. Call 911. It’s not a big deal. It’s the only deal that matters.
jagdish kumar
The brain is a temple. TIA is the whisper before the earthquake. You ignore the whisper, you get the earthquake. No second chances. No do-overs. Just silence.