Serum Sickness-Like Reaction: Causes, Drugs That Trigger It, and What to Do
When your body overreacts to a medicine, it can trigger something called a serum sickness-like reaction, a delayed immune response to certain drugs that mimics the symptoms of classic serum sickness, often caused by animal-derived antiserum. Also known as drug-induced serum sickness, it’s not an allergy in the classic sense—more like your immune system gets confused and starts attacking your own tissues. This isn’t rare. It shows up after taking antibiotics like cefaclor, anticonvulsants like phenytoin, or even biologics used for autoimmune diseases. You might not feel anything for days or even weeks after starting the drug, then suddenly get joint pain, a rash, fever, and swollen lymph nodes.
What makes this reaction tricky is how similar it looks to real serum sickness, which used to come from horse or rabbit antitoxins. Today, it’s almost always drug-related. The key triggers we see in real cases? cefaclor, a second-generation cephalosporin antibiotic commonly prescribed for ear and respiratory infections in kids, is one of the top offenders. Others include minocycline, a tetracycline-class antibiotic used for acne and other bacterial infections, and even allopurinol, a drug for gout that can cause severe immune reactions in some people. These aren’t just side effects—they’re immune system misfires. Symptoms usually start 1 to 3 weeks after starting the drug, and they don’t get better until you stop taking it.
If you’ve been on a new medication and suddenly feel like you’ve got the flu plus a red, itchy rash and achy joints, don’t brush it off. This isn’t a simple case of hives or a stomach bug. It’s your body sending a clear signal: something’s wrong. Stopping the drug is step one. Getting checked by a doctor is step two. Blood tests can show elevated eosinophils or immune complexes, and skin biopsies sometimes confirm the pattern. The good news? Most people recover fully once the drug is out of their system. Steroids might be needed for severe cases, but antibiotics or antihistamines won’t fix it—because it’s not an infection or a classic allergy.
What you’ll find in the posts below is a collection of real-world cases and practical guides on how drugs trigger unexpected immune responses. You’ll see how pediatric patients react differently to antibiotics, why kidney function matters when using certain meds, and how common drugs like ivermectin or voriconazole can cause more than just stomach upset. These aren’t theoretical scenarios—they’re stories from people who got sick after taking something they thought was safe. And if you’ve ever wondered why one person reacts badly to a drug while another doesn’t, the answers are here.
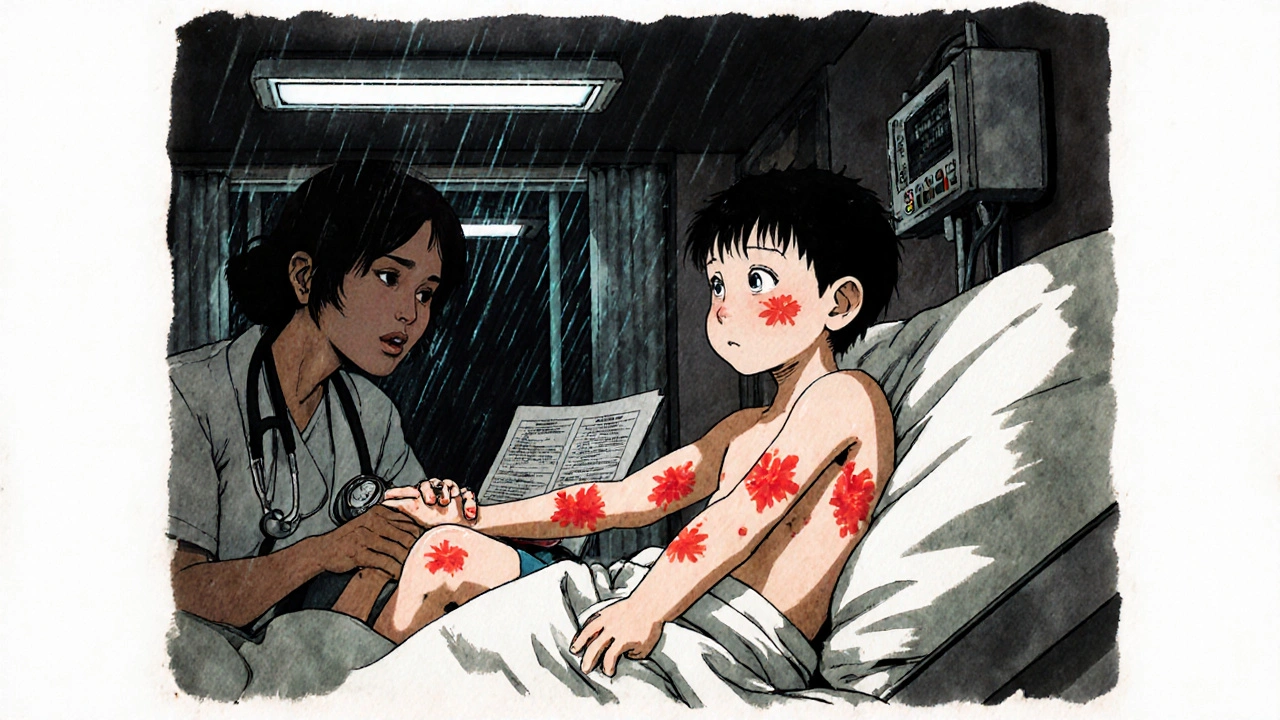
Serum Sickness-Like Reactions to Antibiotics: What Parents and Doctors Need to Know
Serum sickness-like reactions are delayed, non-allergic responses to antibiotics like cefaclor, often mistaken for true allergies. Learn the symptoms, how it's diagnosed, and why avoiding all penicillins is unnecessary.