Myiasis Medication: Treatments, Drugs, and Care
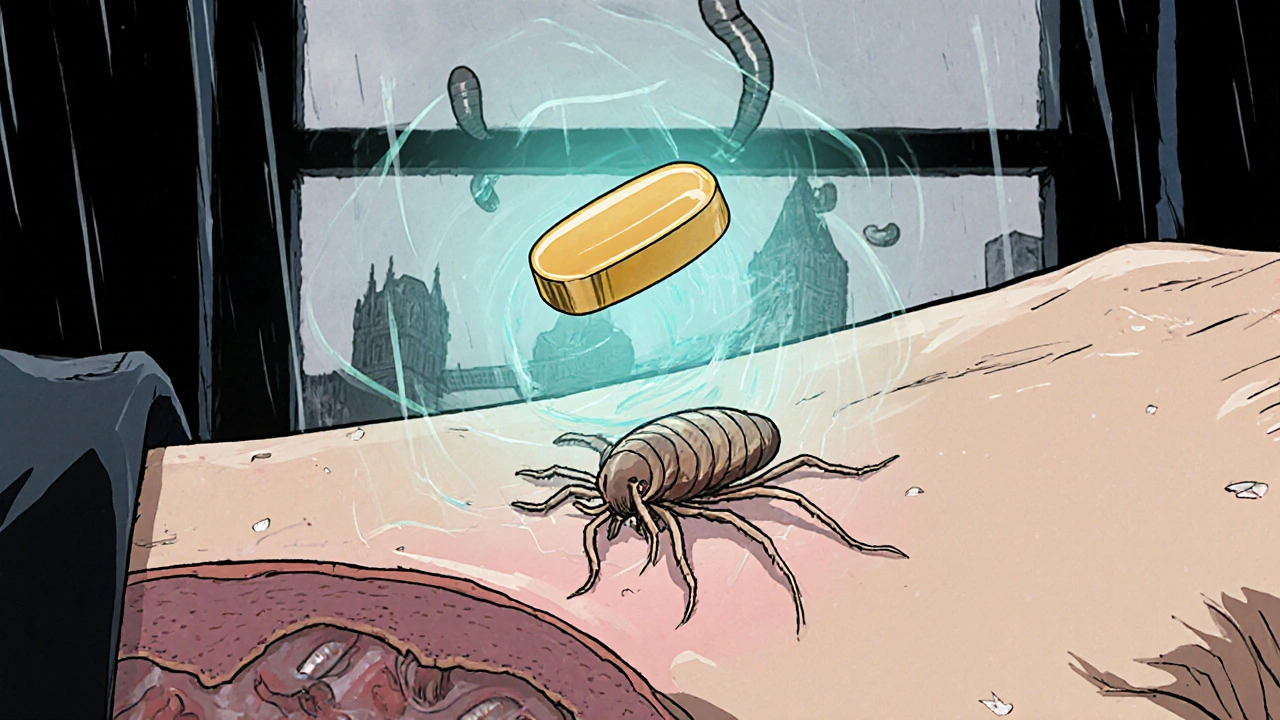
When dealing with myiasis medication, drugs used to eliminate fly‑larvae infestations in human tissue. Also known as larvicidal therapy, it targets the parasites causing the condition and supports healing of the affected area. The condition itself, myiasis, is an infestation of live larvae (maggots) in skin or wounds, and it often requires prompt medical attention. A typical antiparasitic drug, medication that kills or inhibits parasites forms the core of any effective therapy.
myiasis medication isn’t a one‑size‑fits‑all solution; the right choice depends on the type of fly, the depth of infestation, and patient factors like age or allergies.
Key Antiparasitic Options
Most clinicians start with oral agents that have proven activity against a wide range of larvae. Ivermectin, a broad‑spectrum antiparasitic that disrupts nerve signals in insects is often the go‑to drug because it works well for both cutaneous and subcutaneous myiasis. For tougher cases, especially when larvae are deep‑seated, doctors may add topical formulations like permethrin or use systemic drugs such as albendazole, a benzimidazole that interferes with parasite microtubule formation. The choice of drug influences how quickly the larvae die, which in turn affects wound healing speed and infection risk.
Semantic triple: Myiasis medication treats myiasis. Semantic triple: Effective myiasis medication requires an antiparasitic drug. Semantic triple: Choosing the right antiparasitic drug influences wound healing outcomes.
When oral therapy is prescribed, dosing is usually weight‑based, and the treatment length can range from a single dose to a week of daily pills. Side‑effects are generally mild—headache, nausea, or light‑headedness—but patients should be warned about possible allergic reactions, especially if they have a history of drug hypersensitivity.
In addition to medication, proper wound care is essential. Gentle debridement (removing dead tissue) helps expose hidden larvae and improves drug penetration. Clean the area with saline, apply a sterile dressing, and monitor for signs of secondary bacterial infection such as increased redness, pus, or fever. If infection develops, a short course of antibiotics may be added.
Some infestations occur in vulnerable populations—children, the elderly, or people with limited hygiene. For these groups, topical agents like ciclopirox, an antifungal that also has activity against certain larvae can be safer because they avoid systemic exposure. However, topical therapy alone often isn’t enough for deep myiasis, so a combined approach works best.
Prevention is another angle worth mentioning. Reducing exposure to flies by using screens, proper waste management, and wearing protective clothing in endemic areas cuts down the risk dramatically. If you travel to regions where myiasis is common, inspect any skin lesions daily and seek medical help at the first sign of crawling sensations.
Diagnostics may involve a simple visual exam, but in uncertain cases doctors can use ultrasound to locate larvae beneath the skin. Imaging helps decide whether surgical removal is needed, especially for large or necrotic infestations. Imaging also confirms that the chosen medication has reached the target.
Finally, follow‑up matters. After completing the drug regimen, a second wound assessment ensures that no larvae remain and that healing is progressing. If any residual larvae are found, a repeat dose or a different antiparasitic may be required.
Below you’ll find a curated list of articles that dive deeper into specific drugs, compare treatment options, and offer practical tips for managing myiasis in different settings. Whether you’re a healthcare professional or just curious about the best approach, the resources below will give you clear, actionable information.
Ivermectin for Skin Parasites: How to Treat Scabies, Larva Migrans & More
Learn how ivermectin treats skin parasites like scabies, larva migrans, demodex and myiasis, with dosing, safety tips, and a comparison table for scabies treatment.