Dose Adjustment: How to Safely Change Medication Amounts for Better Results
When your body doesn’t respond the way it should to a medication, dose adjustment, the process of changing how much of a drug you take based on your individual needs. Also known as medication titration, it’s not a guess—it’s a science built on how your kidneys process drugs, how old you are, what other pills you’re on, and even your weight. Think of it like tuning a radio: too little signal and you miss the station; too much and you get static. The same goes for your meds.
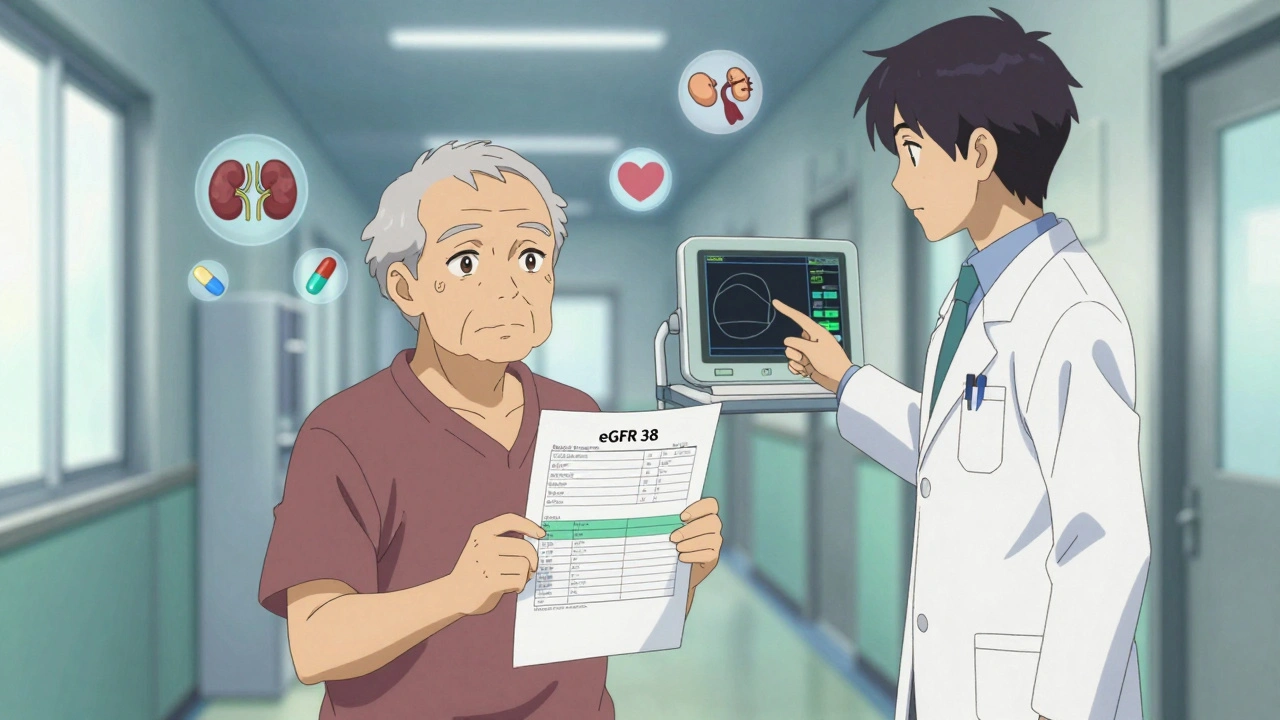
One of the most common reasons for dose adjustment is kidney function, how well your kidneys filter waste and drugs from your blood. Many medications, like metformin or certain antibiotics, are cleared through the kidneys. If your kidneys aren’t working at 100%, those drugs can build up and cause harm. Doctors use tests like eGFR to figure out if you need less, not more. It’s not about being weak—it’s about your body’s unique ability to handle the drug.
Insulin dosing, a precise form of dose adjustment used in diabetes to match food, activity, and blood sugar levels is another everyday example. Basal-bolus insulin isn’t one-size-fits-all. You might need more on days you eat more, less when you’re sick, or none at all if your blood sugar drops too low. That’s dose adjustment in real time. Same goes for blood thinners like warfarin—your dose changes based on lab results, not a fixed number on the bottle.
Drug interactions also force dose changes. If you’re on linezolid, you can’t eat aged cheese or cured meats—not just because of side effects, but because the interaction can spike your blood pressure dangerously. Or take St. John’s Wort: it can make birth control, antidepressants, or transplant drugs stop working by speeding up how fast your liver breaks them down. That’s not a coincidence—it’s a pharmacokinetic shift, and your dose must shift too.
Age matters. Older adults often need lower doses because their bodies process drugs slower. Kids need doses based on weight, not age. And if you’re traveling with refrigerated meds or managing multiple prescriptions, dose adjustment isn’t just clinical—it’s practical. You might need to split pills, change timing, or switch to a different form entirely to stay on track.
It’s not about taking more or less—it’s about taking the right amount for you. Too little and the drug won’t work. Too much and you risk side effects, hospital visits, or worse. That’s why reading FDA safety alerts, using secure messaging with your pharmacist, and understanding your insurance’s copay structure all tie back to one thing: getting your dose right.
Below, you’ll find real guides on how to adjust doses safely—for insulin, kidney patients, seniors, travelers, and anyone juggling multiple meds. No fluff. No theory. Just what works when your life depends on it.
Metformin and Kidney Function: How to Monitor and Adjust Doses Safely
Metformin is safe for most people with type 2 diabetes and mild-to-moderate kidney disease. Learn how eGFR guides dosing, when to hold the drug, and why stopping it unnecessarily can harm your health.