Metformin Dosing Calculator
Metformin Dosing Calculator
Determine the safe metformin dosage based on your kidney function (eGFR). Follows current FDA, ADA, and NICE guidelines.
Metformin is one of the most commonly prescribed diabetes medications in the world. It’s affordable, effective, and has been shown to lower the risk of heart attacks and strokes in people with type 2 diabetes. But for years, doctors avoided prescribing it to patients with kidney problems-out of fear. That fear was based on outdated rules. Today, we know better. Metformin doesn’t damage your kidneys. In fact, stopping it unnecessarily can be more dangerous than keeping it. The real issue isn’t kidney damage-it’s how your body clears the drug. And that’s where monitoring and dose adjustments come in.
Why Kidney Function Matters with Metformin
Metformin leaves your body almost entirely through your kidneys. If your kidneys aren’t working well, the drug can build up in your blood. That doesn’t mean it’s toxic by itself. But if your kidneys suddenly fail-say, from dehydration, infection, or contrast dye used in imaging tests-metformin can accumulate and raise your risk of lactic acidosis. That’s a rare but serious condition where lactic acid builds up in your blood, causing your pH to drop dangerously low.
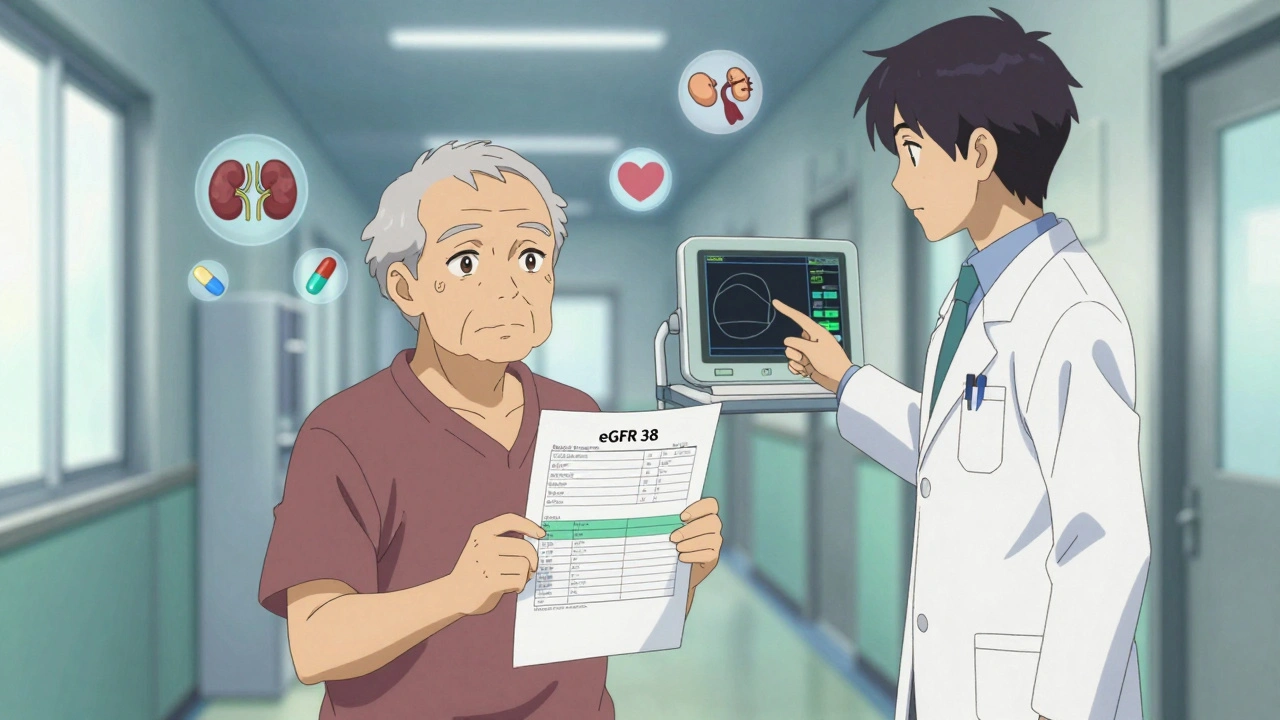
The good news? Lactic acidosis from metformin is extremely rare-only about 3.3 cases per 100,000 people each year. And most of those cases happen when people are already very sick, not because of metformin alone. The bigger problem? Many patients stop taking metformin because they’re told their kidneys are “bad.” That’s a myth. A 2022 study found 22% of eligible patients stopped metformin just because their eGFR dropped below 60-even though they were stable and healthy otherwise. Their blood sugar soared. One 82-year-old’s HbA1c jumped from 6.8% to 8.9% in three months after stopping metformin, all because his eGFR was 38.
What Is eGFR-and Why It’s the New Standard
For decades, doctors used serum creatinine levels to decide if someone could take metformin. Men over 1.5 mg/dL, women over 1.4 mg/dL? No metformin. That was wrong. Creatinine doesn’t tell the full story. It’s influenced by muscle mass, age, and diet. A frail 80-year-old woman might have a “normal” creatinine of 1.2, but her kidneys are barely working. A muscular 40-year-old man might have a creatinine of 1.6, but his kidneys are fine.
That’s why in 2016, the FDA switched to eGFR-estimated glomerular filtration rate. This number estimates how well your kidneys filter waste. It’s calculated using your age, sex, race, and serum creatinine. It’s more accurate. And it changed everything.
Before 2016, metformin was banned if eGFR was below 60. Now? You can still take it if your eGFR is as low as 30. That opened the door for thousands of older adults with mild-to-moderate kidney disease to keep using a drug that protects their heart and helps control their blood sugar.
Dosing Guidelines Based on eGFR
Here’s how dosing works today, based on the latest guidelines from the FDA, ADA, and NICE:
- eGFR ≥60 mL/min/1.73 m²: You can take the full dose-up to 2,550 mg per day. Check kidney function every 6 to 12 months.
- eGFR 45-59 mL/min/1.73 m²: Maximum dose is 2,000 mg per day. Monitor every 3 to 6 months.
- eGFR 30-44 mL/min/1.73 m²: Maximum dose is 1,000 mg per day. Monitor every 3 months. Do not start metformin here unless absolutely necessary. But if you’re already on it and stable, keep going.
- eGFR <30 mL/min/1.73 m²: Metformin is contraindicated. Do not use it. Exceptions? A few experts may consider 500 mg daily in very stable patients with eGFR between 15-30, but this is rare and requires close supervision.
Special cases matter too. If you’re on hemodialysis, take 500 mg after each session. For peritoneal dialysis, 250 mg daily is safe. These are not guesses-they’re based on how much metformin gets removed during each treatment.
When to Hold Metformin
Even if your kidneys are stable, there are times you must pause metformin:
- Before any imaging test with iodinated contrast dye (like a CT scan). If your eGFR is below 60, stop metformin 48 hours before the scan and don’t restart until 48 hours after, once your kidneys are confirmed to be working normally.
- If you’re sick with dehydration, infection, or severe vomiting/diarrhea. Your kidneys can’t handle the extra stress. Hold metformin until you’re back to normal.
- If you’re taking NSAIDs like ibuprofen or naproxen. These can reduce kidney blood flow. Avoid them if your eGFR is below 60.
One common mistake? Patients stop metformin when they’re hospitalized for pneumonia or a UTI-and forget to restart it. That leads to weeks of high blood sugar. Always ask your doctor: “Should I pause my metformin during this illness?”
What About Vitamin B12?
Long-term metformin use-over 4 years-can lower vitamin B12 levels in 7% to 10% of people. That’s not a side effect you feel right away. But low B12 can cause fatigue, numbness in hands and feet, memory problems, and even anemia. It’s easy to miss because it looks like aging or diabetes complications.
Doctors should check your B12 level at least once a year if you’ve been on metformin for more than 4 years. If it’s low, a simple oral supplement or injection fixes it. No need to stop the drug.
What the Guidelines Don’t Agree On
Most guidelines agree on the big picture: eGFR below 30 = stop metformin. But they differ in the gray zone: eGFR 30-45.
- ADA and FDA: Don’t start metformin here, but you can keep using it if you’re already on it and stable.
- AACE/ACE: Reduce the dose and monitor closely.
- NICE (UK): Require a formal dose review whenever eGFR drops below 45.
- KDIGO: Say it’s safe if eGFR is above 45, unless you’re at risk for sudden kidney injury.
Why the confusion? Because real people aren’t numbers. An 80-year-old with eGFR 38 who walks daily, eats well, and takes no other kidney-affecting drugs is very different from a 65-year-old with eGFR 40 who’s on blood pressure meds, drinks alcohol, and skips appointments. The guidelines give you a framework-but your doctor needs to use judgment.
How to Stay Safe: A Simple Monitoring Plan
If you’re on metformin and have kidney disease, here’s what you should do:
- Get your eGFR checked every 3 to 6 months (more often if it’s below 45).
- Ask for your exact eGFR number-not just “your kidneys are okay.” Know your number.
- Keep a log: Write down your eGFR, dose, and any changes in how you feel.
- Stop metformin before any contrast scan and ask when to restart.
- Get your B12 checked yearly after 4 years on metformin.
- Don’t take NSAIDs without checking with your doctor.
- Drink water when you’re sick. Dehydration is the #1 trigger for metformin buildup.
One clinic in Adelaide cut metformin discontinuation by 35% just by teaching patients: “Metformin doesn’t hurt your kidneys. It just needs them to work well to leave your body.” That simple message changed behavior.
The Bigger Picture: Why This Matters
Metformin isn’t just a sugar-lowering drug. It’s a heart protector. The UKPDS trial showed it cuts heart attacks by 32% over 10 years. Newer drugs like SGLT2 inhibitors and GLP-1 agonists are great-but they’re expensive. Metformin costs $4 to $12 a month. It’s still the most prescribed first-line drug in the U.S.-76% of people start with it.
And it’s not going away. Research is ongoing. The MET-FORMIN-CKD trial is now studying whether 500 mg daily is safe and effective for people with eGFR 25-35. Early results are promising. Meanwhile, experts are starting to use cystatin C-a better marker for kidney function in older adults-alongside eGFR to get a clearer picture.
Don’t let outdated myths cost you your health. If your doctor says your kidneys are “too weak” for metformin, ask: “What’s my eGFR? Is it below 30? Am I stable? Can we adjust the dose instead of stopping it?” You might be surprised how many people can-and should-stay on it.
Frequently Asked Questions
Does metformin damage your kidneys?
No, metformin does not damage your kidneys. It’s cleared by your kidneys, but it doesn’t harm them. The old belief that it causes kidney damage is a myth. In fact, stopping metformin unnecessarily can lead to worse blood sugar control and higher heart disease risk. Many patients stop taking it when their eGFR drops below 60-even though guidelines say it’s safe down to eGFR 30.
What should my eGFR be to take metformin?
You can take metformin if your eGFR is 30 mL/min/1.73 m² or higher. For eGFR 30-44, the max dose is 1,000 mg per day. For eGFR 45-59, you can take up to 2,000 mg. At eGFR 60 or higher, you can take the full dose of 2,550 mg. Metformin is not recommended if your eGFR is below 30, unless under very close supervision.
When should I stop metformin before a CT scan?
If your eGFR is below 60, stop metformin 48 hours before a CT scan that uses iodinated contrast dye. Do not restart it until 48 hours after the scan, and only after your kidney function has been checked and confirmed to be stable. This prevents contrast-induced kidney injury from combining with metformin buildup.
Can I take metformin if I’m on dialysis?
Yes, but with specific dosing. If you’re on hemodialysis, take 500 mg after each dialysis session. If you’re on peritoneal dialysis, 250 mg once daily is safe. Your body removes metformin during dialysis, so timing matters. Never take your full pre-dialysis dose without adjusting.
Why am I being checked for vitamin B12?
Long-term metformin use-usually over 4 years-can lower vitamin B12 levels in 7-10% of people. Low B12 can cause fatigue, nerve tingling, memory issues, and anemia. It’s easy to mistake for diabetes complications. Get your B12 checked yearly if you’ve been on metformin for more than 4 years. If it’s low, a simple supplement fixes it without stopping the drug.
Justin Hampton
Yeah right, like metformin is some miracle drug. I’ve seen too many old folks on it with creatinine levels that should’ve banned them, then end up in the ER with acidosis. Doctors are too lazy to think anymore-they just follow guidelines like robots. If your kidneys are barely working, stop the metformin. Period.
Pooja Surnar
omg this is so true!! i had my uncle on metformin and his creatinine was 2.1 and dr still kept him on it!! he got so weak and confused!! its not about eGFR its about real kidney function!! who even trusts these fancy numbers?? my aunt in delhi got her kidney tested with ultrasound and they said no metformin!! why dont us doctors listen to real life??
Sandridge Nelia
This is such a clear, well-researched breakdown-thank you! 🙏 I’m a nurse and I’ve seen so many patients panic when their eGFR drops to 48 and get told to stop metformin. The B12 point is CRUCIAL-so many people think their fatigue is just aging, but it’s often deficiency. I always check it at the 4-year mark. Also, hydration during illness is the #1 thing patients overlook. Simple, but life-saving.
Pamela Mae Ibabao
Let’s be real-this post is basically pharma marketing dressed up as medical advice. The ‘lactic acidosis is rare’ line? Sure, if you ignore the 2018 JAMA study that showed a 3x higher risk in eGFR 30-44 patients on full doses. And don’t get me started on the ‘metformin protects your heart’ myth-it’s correlation, not causation. SGLT2 inhibitors do the same thing without the kidney risks. Why are we clinging to a 60-year-old drug like it’s gospel?
Gerald Nauschnegg
Wait wait wait-so if I’m 72, eGFR 35, and I’ve been on metformin for 12 years with perfect HbA1c, you’re telling me I can keep taking 1000mg? But if I’m 45 with the same numbers and just started, I can’t? That’s insane. Who decided that? Some committee in a room with no patients? My grandma’s on it and she hikes every weekend. Her kidneys are fine. Stop overcomplicating this.
Palanivelu Sivanathan
So… let me get this straight… we’re supposed to trust a number… eGFR… that’s calculated from a formula… that uses RACE… which is a SOCIAL CONSTRUCT… to decide if a human being… gets to live… without diabetes complications…?!!! That’s not medicine… that’s algorithmic colonialism… we’re reducing life to a spreadsheet… and calling it science…
Joanne Rencher
Ugh, another one of these ‘metformin is fine’ rants. I’ve been on it since 2015. My eGFR’s been 38 for three years. My doctor said ‘keep going’. I didn’t ask why. Now I’m tired all the time, my feet are numb, and my B12’s half what it should be. So yeah, I’m on it. But I’m also miserable. And no one told me about the B12 thing until I Googled it. Thanks for the info, I guess.
Erik van Hees
You missed the most important point: cystatin C. eGFR based on creatinine is garbage in older adults, especially women and non-muscular people. I’ve had patients with eGFR 40 but cystatin C showing true GFR of 65. They were denied metformin. Meanwhile, someone with eGFR 55 but high creatinine from bodybuilding gets full dose. That’s not medicine-that’s statistical nonsense. Push for cystatin C testing if you’re over 60. It’s not expensive, and it’s way more accurate.
Cristy Magdalena
I just want to say… this post made me cry. Not because I’m emotional… but because I’ve spent the last two years watching my mother be told she couldn’t take metformin anymore… just because her eGFR dropped to 32… after she’d been stable for 8 years… She cried when she stopped it. Her sugar went wild. Her heart started acting up. And now… she’s on three new drugs… that cost $800 a month… and she’s still tired… and scared… I wish someone had told us this before…
Adrianna Alfano
My dad’s from Nigeria and he’s been on metformin since 2010. His eGFR is 36. He doesn’t speak much English, so when his doctor said ‘your kidneys are bad’, he thought he had to stop everything. I had to translate the guidelines for him. He cried because he thought he was failing. But now he’s back on 500mg and his sugar’s better than ever. We also got his B12 checked-it was 180. He’s on supplements now. This post? It’s the kind of thing that saves lives… especially for people who don’t have a daughter who can Google for them.