Antibiotic Hypersensitivity: Signs, Risks, and What to Do Next
When your body overreacts to an antibiotic hypersensitivity, an immune system response to an antibiotic that goes beyond normal side effects. Also known as drug allergy, it’s not just a rash or upset stomach—it can be life-threatening. This isn’t the same as a side effect like nausea or dizziness. Hypersensitivity means your immune system sees the antibiotic as a threat and attacks it, triggering symptoms that range from mild to severe.
Some of the most common triggers are penicillin, a widely prescribed antibiotic class that causes the majority of reported allergic reactions, and sulfa drugs, like Bactrim, which can cause skin rashes or more serious reactions in sensitive people. Even if you’ve taken an antibiotic before without issues, you can develop hypersensitivity later. It doesn’t matter if you’ve used it five times safely—number six could be the one that triggers a reaction. That’s why doctors don’t just assume you’re safe because you’ve used it before.
Signs you’re having a true allergic reaction include hives, swelling of the face or throat, trouble breathing, wheezing, or a drop in blood pressure. These usually show up within minutes to hours after taking the drug. Less severe reactions—like a delayed rash or fever—can appear days later. If you’ve ever had a reaction, write it down: which drug, what happened, when. That info saves lives. Many people think they’re allergic to penicillin because they got a rash as a kid, but up to 90% of them aren’t truly allergic when tested. Getting checked can open up safer, cheaper treatment options later.
What you avoid matters just as much as what you take. If you’re allergic to one antibiotic, you might need to avoid others in the same family. But not always. Some reactions are specific to one drug, not the whole class. That’s why knowing the exact drug and reaction helps your doctor pick a safe alternative. For example, if you reacted to amoxicillin, you might still be able to take azithromycin or doxycycline—depending on the type of reaction.
People who’ve had antibiotic hypersensitivity are often stuck with less effective or more expensive drugs. That’s why understanding your reaction isn’t just about avoiding danger—it’s about getting the best care possible. If you’ve ever been told you’re allergic to an antibiotic, don’t just accept it. Ask: Was it tested? Could it be a side effect? Could you outgrow it? The answers could change how you’re treated next time you’re sick.
In the posts below, you’ll find real-world stories and comparisons about antibiotics that commonly cause reactions, how to tell the difference between a true allergy and a side effect, and what to do if you’ve been labeled allergic without proper testing. You’ll also see how some drugs like Bactrim or tetracycline show up in reactions, and what alternatives work when you can’t use the usual options. This isn’t just theory—it’s what people actually face when their body says no to a medicine they thought was safe.
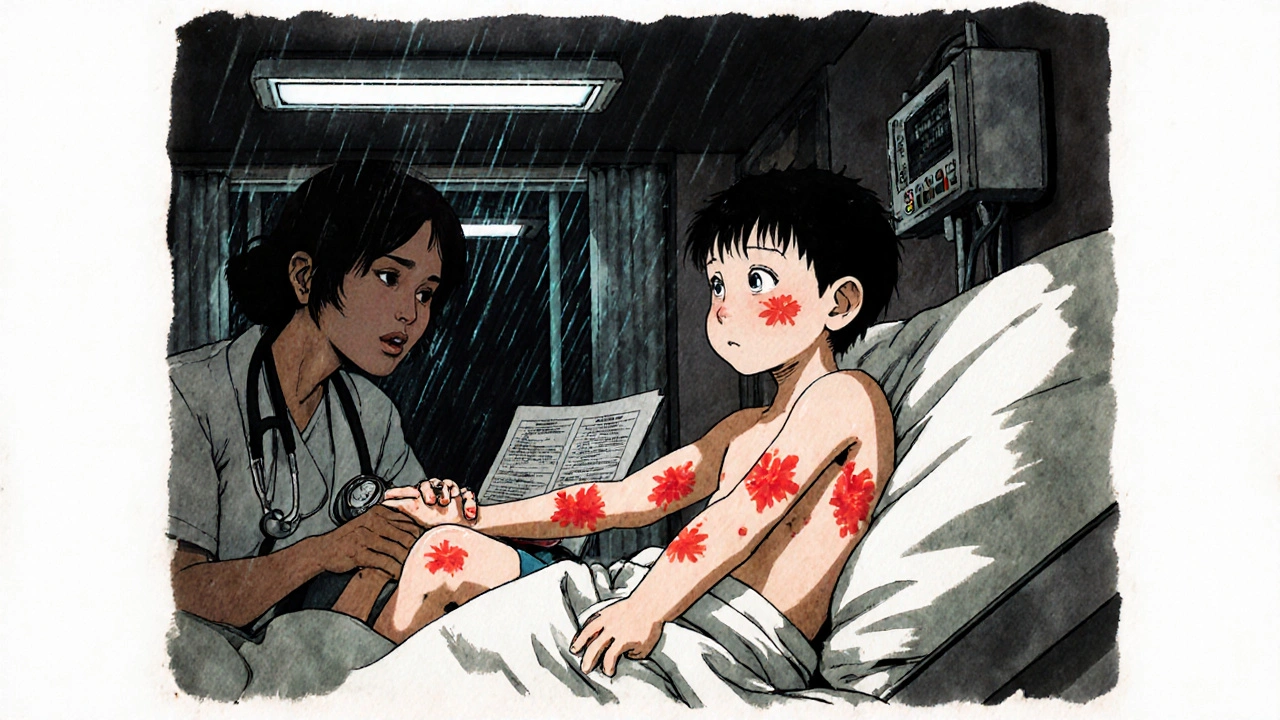
Serum Sickness-Like Reactions to Antibiotics: What Parents and Doctors Need to Know
Serum sickness-like reactions are delayed, non-allergic responses to antibiotics like cefaclor, often mistaken for true allergies. Learn the symptoms, how it's diagnosed, and why avoiding all penicillins is unnecessary.