When you’re pregnant or breastfeeding and have asthma, the last thing you want to do is harm your baby. But the truth is, uncontrolled asthma is far more dangerous than the medications you use to manage it. Many women stop their inhalers out of fear - and that’s when things get risky. If you can’t breathe, your baby can’t breathe either. Oxygen levels drop for both of you. The risk of preterm birth, low birth weight, or preeclampsia goes up. Studies show that women with poorly controlled asthma during pregnancy are 30-40% more likely to have complications than those who keep their asthma under control with medication.
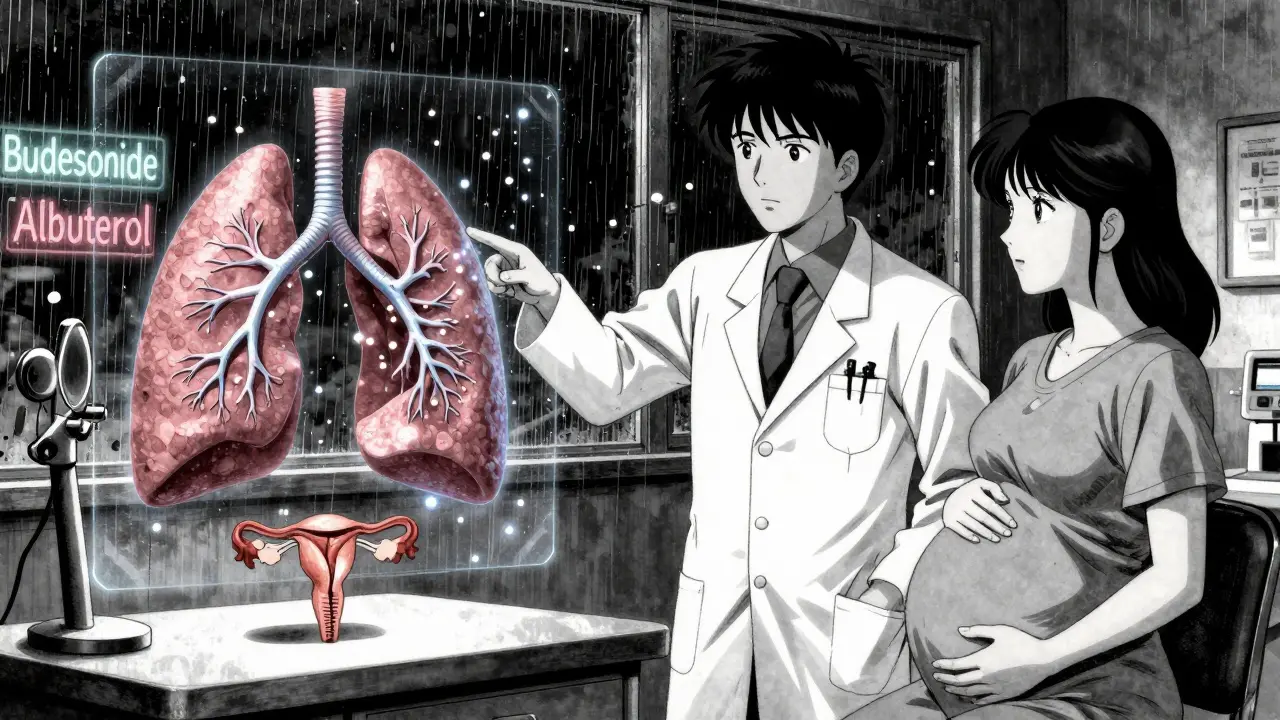
Most Asthma Medications Are Safe - Especially Inhalers
The biggest myth is that all asthma drugs are risky during pregnancy or breastfeeding. That’s not true. Inhaled medications - the kind you use in your inhaler - are the gold standard. Why? Because they go straight to your lungs. Only 10-30% of the dose even enters your bloodstream. The rest gets coughed out or stays in your airways. That means almost nothing reaches your baby.
Take budesonide (Pulmicort), one of the most studied inhaled corticosteroids. Over 10,000 pregnancy outcomes have been tracked, and there’s no link to birth defects. The American College of Obstetricians and Gynecologists says it’s safe. So does the American Lung Association. Even the Better Health Channel in Australia confirms it: using your inhaler as prescribed is safer than going without.
Short-acting bronchodilators like albuterol (Ventolin) are just as safe. These are your rescue inhalers - the ones you use when you feel tightness or wheezing. National Jewish Health reviewed data from thousands of pregnant women and found no increase in birth defects, even at standard doses. You don’t need to cut back. You don’t need to wait until after feeding. Just use it when you need it.
What About Oral Medications and Pills?
Oral steroids like prednisone are a different story. They enter your bloodstream more fully, so they’re used more cautiously. But even then, they’re not off-limits. If your asthma flares badly - say, during a severe infection or an asthma attack - your doctor might prescribe a short course of oral steroids. The Breastfeeding Network says that if you take 40mg of prednisolone for five days or less, it’s unlikely to affect your baby. For higher doses, you might be advised to wait a few hours after taking the pill before breastfeeding, or pump and discard milk once. That’s it.
Other oral medications like theophylline are still used, but they require monitoring. Blood levels need to be checked regularly because your body processes them differently during pregnancy. That’s why doctors usually avoid these unless absolutely necessary. The American Academy of Allergy, Asthma & Immunology says clearly: “Oral medications (pills) should be avoided unless necessary.” Stick to inhalers first. Always.
Breastfeeding and Asthma Medications: No Need to Worry
Many new moms panic about whether their asthma meds will get into breast milk. The answer? Almost none of them do - in meaningful amounts.
Inhaled corticosteroids? Less than 0.1% of the dose ends up in breast milk. That’s less than what’s in a drop of water. Albuterol? Same thing. The Breastfeeding Network in the UK states plainly: “Asthma inhalers do not produce levels of drug in the blood system let alone in milk, so are safe to use as normal.” No timing adjustments. No pumping and dumping. Just use your inhaler like you always have.
Even prednisolone - the oral steroid - transfers at only 5-25% of your blood concentration. And that’s still far below what’s given to newborns for medical conditions. Montelukast (Singulair), the leukotriene blocker, shows up in milk in tiny amounts - less than what’s in a baby’s daily dose for asthma. It’s not a concern.
There’s one exception: theophylline. It does transfer more noticeably. But even then, studies show infant blood levels stay well below the therapeutic range. Still, if you’re on theophylline and breastfeeding, your doctor may monitor your baby for irritability or poor feeding. Most moms never see an issue.
What About Newer Biologics Like Xolair or Nucala?
This is where things get trickier. Drugs like omalizumab (Xolair), mepolizumab (Nucala), and dupilumab (Dupixent) are powerful, but they’re relatively new. There’s not enough data yet on how they affect babies during pregnancy or breastfeeding.
The FDA still lists them as Category B - meaning animal studies show no harm, but human data is limited. The American Academy of Allergy, Asthma & Immunology says this clearly: “Less experience exists with newer agents during breastfeeding.” If you’re already on one of these and get pregnant, don’t stop cold turkey. Talk to your doctor. They may recommend staying on it if your asthma is severe, or switching to something with more safety data.
Right now, the NIH is funding a $4.7 million registry to track 5,000 pregnancies in women using biologics. Results won’t be available until 2027. Until then, use these only if your asthma is uncontrolled on standard treatments - and only under close supervision.
What Happens When You Stop Your Medication?
One in five pregnant women with asthma stops or cuts back on their meds because they’re scared. The Asthma and Allergy Foundation of America found that 22% of pregnant asthmatics reduce or stop their inhalers without talking to a doctor. The result? A 37% spike in emergency room visits compared to those who stayed on their treatment.
One study followed 327 pregnant women with asthma who stuck to their inhalers. 98.7% delivered full-term babies with normal birth weights. In the group that stopped or skipped meds? Only 76.4% had normal birth weights. That’s a massive difference.
And it’s not just about the baby. Uncontrolled asthma increases your risk of preeclampsia, hospitalization, and even ICU admission. You’re not just protecting your child - you’re protecting yourself.

How to Stay Safe: A Simple Action Plan
Here’s what you should do right now, whether you’re trying to get pregnant, already pregnant, or breastfeeding:
- See your doctor before conception - or as soon as you find out you’re pregnant. Don’t wait. Get your asthma action plan updated.
- Keep using your inhalers - both controller (daily) and rescue (as needed). No exceptions.
- Monitor your breathing - use a peak flow meter at home. Your lung capacity drops slightly in late pregnancy - that’s normal. But if your peak flow drops below your personal baseline by 20%, call your doctor.
- Check in every 4-6 weeks - pregnant women need more frequent asthma check-ups than non-pregnant ones.
- Don’t mistake normal pregnancy breathlessness for asthma - 60-70% of pregnant women feel short of breath in the third trimester, even if they don’t have asthma. If your inhaler doesn’t help, it’s probably not asthma.
- Never stop meds without talking to your doctor - even if you feel fine. Asthma can flare without warning.
What to Do If You’re Still Scared
It’s okay to be scared. You’re not alone. Reddit threads like r/asthma have hundreds of posts from moms terrified to use their inhalers. But the data doesn’t lie. The risks of stopping are real. The risks of using inhalers? Nearly zero.
Ask your doctor for printed materials from the American Lung Association or the Better Health Channel. Read the studies. Talk to other moms. You’ll find that most women who stayed on their meds had healthy pregnancies and healthy babies.
Remember: “Asthma medicine will not harm your baby. Taking medicine is safer for you and your baby than having asthma that is not under control.” That’s not a slogan - it’s science.
What’s Changing in 2025?
More doctors are getting trained on asthma care during pregnancy. Kaiser Permanente’s Pregnancy Asthma Protocol reduced preterm births by 28% after it rolled out in 2021. More OB-GYNs are now working with pulmonologists to create joint care plans.
The FDA’s Pregnancy and Lactation Labeling Rule (PLLR), which replaced old letter categories (A, B, C, D, X), now requires drug labels to include clearer summaries of risks and benefits. All major asthma medications have been updated by 2018 - so your prescription label should give you honest, detailed info.
By 2030, experts predict 95% of pregnant asthmatics will stay on their meds - up from 75% today. Why? Because education is working. More women are learning the truth: your inhaler isn’t the danger. Your asthma is.

Tony Du bled
Just wanted to say this post saved my life. I stopped my inhaler in my first trimester because I was terrified. Ended up in the ER with a severe attack. My OB looked me dead in the eye and said, 'You’re not protecting your baby by choking.' I started back on budesonide and never looked back. Baby’s 2 now, healthy as a horse.
Kathryn Weymouth
The data cited here is exceptionally well-sourced and rigorously presented. The distinction between inhaled corticosteroids and oral systemic agents is clinically significant and accurately conveyed. Particularly noteworthy is the emphasis on the negligible transfer of medication into breast milk, which is supported by pharmacokinetic studies published in the Journal of Allergy and Clinical Immunology. This post represents a model of evidence-based patient education.
Herman Rousseau
YES. This. So many moms panic and quit their meds like it’s some kind of detox. I was one of them. Then I met a nurse midwife who said, 'Your baby doesn’t care if your inhaler is synthetic-it cares if you can breathe.' I started using my albuterol like a normal human again. No pumping, no waiting, no guilt. My daughter’s five, plays soccer, and has never had asthma. That’s the win.
Candy Cotton
It is both scientifically inaccurate and dangerously irresponsible to suggest that pharmaceutical intervention during gestation is without consequence. The FDA’s own labeling protocols, while improved, remain insufficiently granular to account for individual genetic variability in placental transfer. Furthermore, the normalization of pharmacological dependence during lactation undermines the natural biological imperative to minimize xenobiotic exposure. One must exercise extreme caution, even if the majority of outcomes appear favorable.
Gabriella da Silva Mendes
Okay but like… why is everyone so scared of pills? I took prednisone for 3 days when I had a bad flare and I still breastfed. My baby didn’t turn into a tiny dragon. He just slept more and pooped like a champ. Also, I used my inhaler while eating tacos at 2am and nothing exploded. Like… are we really this scared of medicine now? I get it, but also-my lungs were on fire and I didn’t want to die in a Target parking lot. So I used my meds. And my kid is fine. Like, really fine. Like, plays piano and hates broccoli fine. 🤷♀️
Kiranjit Kaur
As a mom from India who used inhalers during pregnancy, I want to say: your body knows what it needs. I was told by my auntie that 'asthma medicine is poison for the baby'-but my doctor showed me the numbers. I used Pulmicort daily. My daughter is now 3, no allergies, no issues. Don’t listen to grandma’s advice if it’s not backed by science. You’re not being selfish-you’re being smart. 💪❤️
Sai Keerthan Reddy Proddatoori
They say inhalers are safe. But who funds these studies? Big Pharma. They want you dependent. The real danger is breathing polluted city air. Stop blaming medicine. Start blaming the chemicals in your air, your water, your food. The government won’t tell you this. But if you stop the inhaler and live clean-organic food, no AC, walk to work-you’ll heal naturally. I did. My kid never got sick. Trust nature, not pills.
Sam Black
I remember sitting in my OB’s office, trembling because I’d just been diagnosed with asthma and was 8 weeks along. I asked if I could ever be a ‘normal’ mom. She smiled and said, ‘You already are.’ She handed me a pamphlet from the Lung Association with a quote: ‘Your inhaler isn’t the enemy. Your fear is.’ I cried. Then I filled my prescription. Four years later, my daughter still hugs my inhaler like it’s a stuffed animal. She says, ‘It’s my breathing superhero.’ I’m not just a mom-I’m a survivor. And I didn’t survive by holding my breath.