UTI Treatment Options: What Works and Why
When dealing with UTI treatment options, strategies that clear a urinary tract infection (UTI) and prevent recurrence. Also known as urinary infection therapies, they range from prescription antibiotics to home‑based remedies. Understanding how these options fit together helps you pick the safest, fastest path to relief.
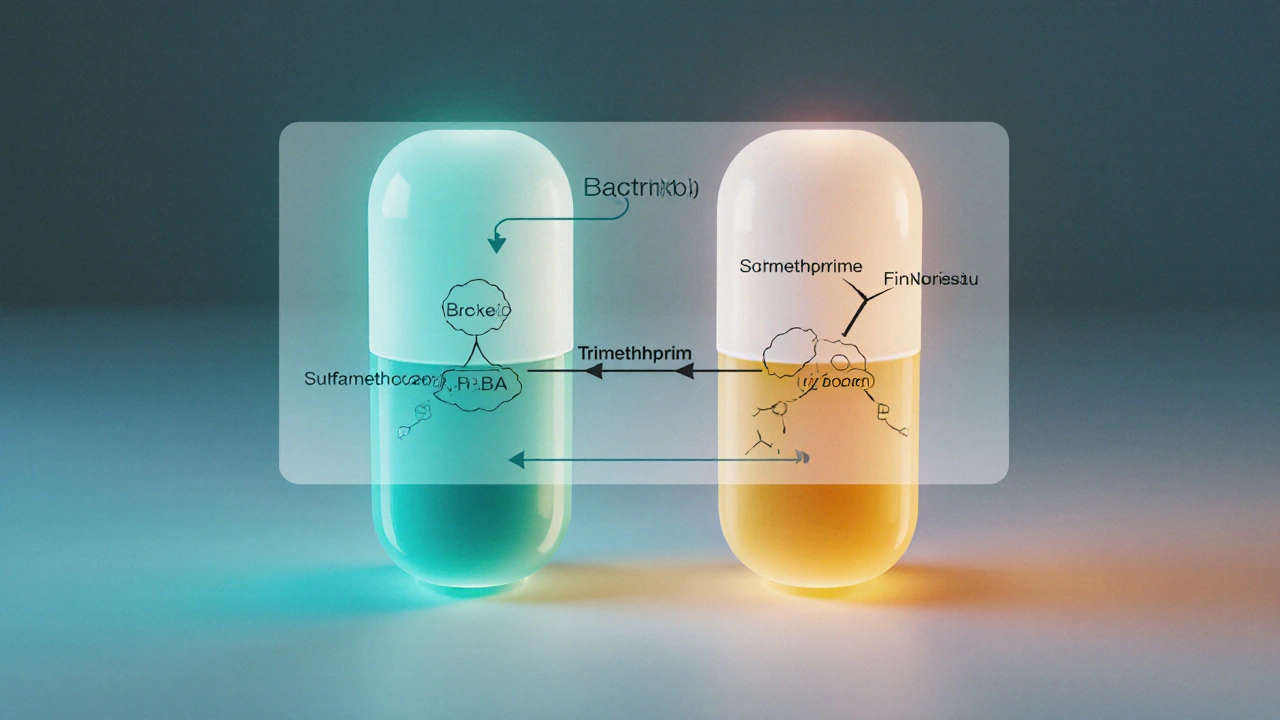
One of the core antibiotics, medications that kill or stop the growth of the bacteria causing the infection is a first‑line treatment for most UTIs. Drugs like trimethoprim‑sulfamethoxazole, nitrofurantoin, and fosfomycin target the typical culprits—E. coli and other gram‑negative bacteria—while minimizing side effects. However, rising antibiotic resistance means doctors now check local resistance patterns before prescribing. If the bacteria are resistant, they may switch to a broader‑spectrum agent such as ciprofloxacin, but that comes with higher risk of gut flora disruption and tendon issues.
Beyond antibiotics, many patients explore alternative therapies, non‑antibiotic approaches that support the urinary system and reduce symptoms. Cranberry juice, D‑mannose supplements, and probiotics are among the most studied. Cranberries contain proanthocyanidins that prevent bacteria from sticking to the bladder wall, while D‑mannose provides a simple sugar that blocks bacterial adhesion. Probiotic strains like Lactobacillus rhamnosus help restore healthy vaginal flora, which can lower the chance of reinfection. Though these methods rarely replace antibiotics for acute infections, they’re valuable for prevention and for people who can’t tolerate standard drugs.
When to Choose Each Option
Choosing the right bacterial infection, infection caused by pathogenic bacteria in the urinary tract treatment depends on three factors: symptom severity, infection history, and personal health conditions. Mild symptoms (burning, urgency) that appear early often respond well to a short course of a narrow‑spectrum antibiotic. Recurrent infections—three or more per year—might need a longer prophylactic regimen or a switch to non‑antibiotic strategies like daily D‑mannose. Pregnant women, diabetics, and patients with kidney stones require special care; certain antibiotics are unsafe in pregnancy, while others can be cleared faster in patients with impaired kidney function.
Another key decision point is the setting: outpatient versus hospital. Complicated UTIs that involve the kidneys (pyelonephritis) or cause fever typically need IV antibiotics and close monitoring. Simple cystitis, which stays in the bladder, can be managed at home with oral meds and supportive care. Because each case varies, discussing symptom duration, prior drug reactions, and any allergies with your provider ensures the chosen regimen is both effective and safe.
In practice, a blended approach works best. Start with an evidence‑based antibiotic to quickly reduce bacterial load, then add an alternative therapy to reinforce bladder health and prevent future episodes. Keep hydrated, empty your bladder regularly, and avoid irritants like caffeine or alcohol—simple habits that boost the effectiveness of any treatment plan.
Below you’ll find a curated list of articles that dive deeper into each of these aspects. From detailed antibiotic comparisons to step‑by‑step guides on buying generic meds safely, the collection equips you with the knowledge you need to manage UTIs confidently and cost‑effectively.
Bactrim vs Alternatives: Which Antibiotic Fits Your Needs?
Compare Bactrim with five common alternatives, see side‑effects, dosing, and when each drug is the best choice.