Bactrim vs Alternatives: Antibiotic Selector
Select Your Scenario
Choose your infection type, patient factors, and preferences to get personalized antibiotic recommendations.
Recommended Antibiotic
Why This Choice?
Antibiotic Comparison Table
| Drug | Spectrum | Typical Indications | Dosage Frequency | Common Side Effects | Resistance Concerns |
|---|---|---|---|---|---|
| Bactrim | Broad (Gram-positive & Gram-negative) | UTI, respiratory, PCP prophylaxis | Twice daily | Kidney strain, photosensitivity | Increasing E. coli resistance in some regions |
| Doxycycline | Broad, good for atypicals | Respiratory, acne, some UTIs | Once or twice daily | GI upset, photosensitivity | Low resistance in community-acquired infections |
| Azithromycin | Moderate, strong against atypicals | Sinusitis, bronchitis, chlamydia | Once daily for 3-5 days | QT prolongation, mild GI upset | Rising macrolide resistance in S. pneumoniae |
| Ciprofloxacin | Strong Gram-negative, some Gram-positive | Complicated UTI, prostatitis, abdominal infections | Twice daily | Tendonitis, CNS effects | High resistance in certain Enterobacteriaceae |
| Nitrofurantoin | Urine-concentrated, limited systemic | Uncomplicated cystitis | Twice daily | Pulmonary issues, nausea | Rare resistance; effectiveness maintained |
| Amoxicillin-clavulanate | Broad, beta-lactamase coverage | Sinusitis, otitis media, skin infections | Three times daily | Diarrhea, liver enzyme changes | Beta-lactamase producers may still resist |
Key Takeaways
- Bactrim combines sulfamethoxazole and trimethoprim to block bacterial folate synthesis.
- Common alternatives include doxycycline, azithromycin, ciprofloxacin, nitrofurantoin, and amoxicillin‑clavulanate.
- Choosing the right drug depends on infection type, kidney function, allergy history, and local resistance patterns.
- Side‑effect profiles differ: Bactrim can cause kidney strain, while fluoroquinolones may trigger tendon issues.
- Always confirm dosage and duration with a clinician, especially for pregnant patients or those with chronic illnesses.
What Is Bactrim?
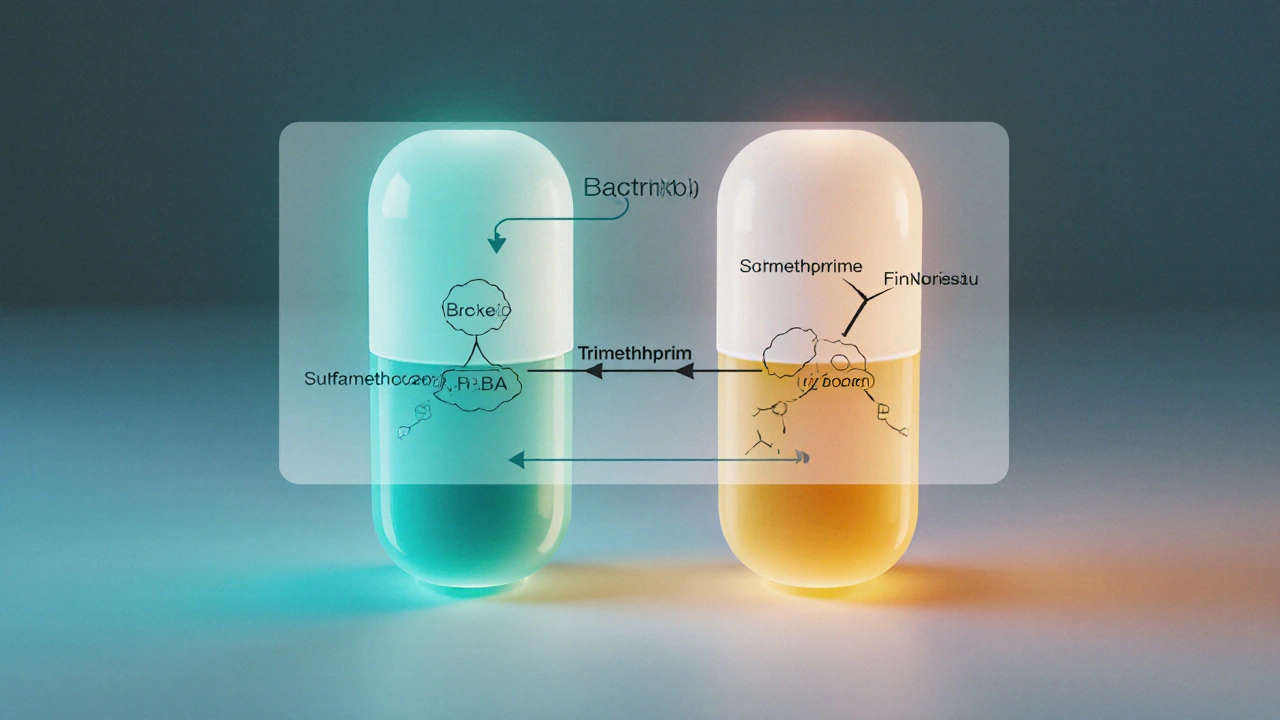
When doctors prescribe Bactrim (sulfamethoxazole/trimethoprim), they’re using a fixed‑dose combo that hits two steps in bacterial folate production. The first component, sulfamethoxazole, belongs to the sulfonamide class and mimics para‑aminobenzoic acid. The second, trimethoprim, blocks dihydrofolate reductase. Together they create a synergistic effect that makes resistance harder for bacteria to develop.
Typical uses include uncomplicated urinary tract infections (UTIs), certain respiratory infections, and prophylaxis for Pneumocystis jirovecii pneumonia in immunocompromised patients.
How Bactrim Works
The sulfonamide component competes with PABA, preventing synthesis of dihydropteroic acid, while trimethoprim stops conversion of dihydrofolic acid to tetrahydrofolic acid. Without tetrahydrofolic acid, bacterial DNA can’t be replicated, leading to cell death. Because the two drugs hit consecutive steps, the combo often clears infections faster than either agent alone.

When to Consider an Alternative
Even a powerful combo isn’t perfect. Clinicians look for red flags before clicking Bactrim on the prescription pad:
- Severe kidney impairment (eGFR<30mL/min/1.73m²) - Bactrim is cleared renally and can build up.
- Known sulfa allergy - patients who react to sulfonamides may develop rash or Stevens‑Johnson syndrome.
- Pregnancy, especially in the first trimester - trimethoprim is a folate antagonist that can affect fetal development.
- High local resistance rates - some regions report >30% resistance among E.coli isolates.
- Need for once‑daily dosing - Bactrim usually requires twice‑daily administration.
In these scenarios, doctors turn to alternatives that match the infection’s spectrum while sidestepping the specific concern.
Top Alternatives at a Glance
Below are five widely used antibiotics that often replace Bactrim. Each entry includes the drug’s class, typical dose, and a quick look at side effects.
- Doxycycline - a tetracycline class, taken once or twice daily, common for respiratory infections and some UTIs.
- Azithromycin - a macrolide, favored for its three‑day regimen and good activity against atypical pathogens.
- Ciprofloxacin - a fluoroquinolone, powerful for complicated UTIs and gram‑negative infections.
- Nitrofurantoin - a nitrofuran, highly concentrated in urine, ideal for uncomplicated cystitis.
- Amoxicillin‑clavulanate - a beta‑lactam combo, broad spectrum including many beta‑lactamase‑producing organisms.
Side‑Effect Snapshot
Understanding adverse‑event patterns helps you weigh benefits against risks. Below is a concise side‑effect profile for each drug.
- Bactrim - kidney‑related electrolyte shifts, photosensitivity, rare blood dyscrasias.
- Doxycycline - gastrointestinal upset, photosensitivity, tooth discoloration in children.
- Azithromycin - mild GI upset, QT‑prolongation risk when combined with certain meds.
- Ciprofloxacin - tendonitis, CNS effects (dizziness, confusion), possible drug‑drug interactions via CYP1A2.
- Nitrofurantoin - pulmonary fibrosis with long‑term use, nausea, hemolysis in G6PD deficiency.
- Amoxicillin‑clavulanate - diarrhea, liver enzyme elevation, allergic rash.
Comparison Table
| Drug | Spectrum | Typical Indications | Dosage Frequency | Common Side Effects | Resistance Concerns |
|---|---|---|---|---|---|
| Bactrim | Broad (Gram‑positive & Gram‑negative) | UTI, respiratory, PCP prophylaxis | Twice daily | Kidney strain, photosensitivity | Increasing E. coli resistance in some regions |
| Doxycycline | Broad, good for atypicals | Respiratory, acne, some UTIs | Once or twice daily | GI upset, photosensitivity | Low resistance in community‑acquired infections |
| Azithromycin | Moderate, strong against atypicals | Sinusitis, bronchitis, chlamydia | Once daily for 3‑5 days | QT prolongation, mild GI upset | Rising macrolide resistance in S. pneumoniae |
| Ciprofloxacin | Strong Gram‑negative, some Gram‑positive | Complicated UTI, prostatitis, abdominal infections | Twice daily | Tendonitis, CNS effects | High resistance in certain Enterobacteriaceae |
| Nitrofurantoin | Urine‑concentrated, limited systemic | Uncomplicated cystitis | Twice daily | Pulmonary issues, nausea | Rare resistance; effectiveness maintained |
| Amoxicillin‑clavulanate | Broad, beta‑lactamase coverage | Sinusitis, otitis media, skin infections | Three times daily | Diarrhea, liver enzyme changes | Beta‑lactamase producers may still resist |
Pros and Cons of Each Option
Summarizing the table helps you match a drug to a patient profile.
- Bactrim: great for mixed Gram‑positive/negative infections; downside is renal dosing and sulfa allergy risk.
- Doxycycline: convenient once‑daily dosing, works on atypicals; not ideal for pregnant women or young children.
- Azithromycin: short course boosts adherence; watch for heart rhythm issues.
- Ciprofloxacin: powerful for resistant gram‑negatives; avoid in patients with tendon problems.
- Nitrofurantoin: stays in urine, low systemic side effects; unsuitable for kidney dysfunction (eGFR<60).
- Amoxicillin‑clavulanate: covers beta‑lactamase producers; higher pill burden and GI upset.
Choosing the Right Antibiotic - A Quick Decision Guide
- Identify the infection site (urinary, respiratory, skin, etc.).
- Check patient’s renal function and allergy history.
- Look up local antibiogram data for common pathogens.
- Match the drug’s spectrum to the likely organism.
- Consider dosing convenience and adherence factors.
- Review side‑effect profile against patient comorbidities.
If a patient has a sulfa allergy, skip Bactrim and lean toward doxycycline or azithromycin for uncomplicated cases. For a pregnant woman with a UTI, nitrofurantoin (if kidneys are fine) or amoxicillin‑clavulanate are safer bets. When resistance is high, ciprofloxacin may be the only oral option, but only after confirming no tendon risk.
Next Steps & Troubleshooting
After the prescription, monitor for two weeks to catch any delayed adverse events. If the infection isn’t improving within 48‑72hours, reassess culture results and consider switching to a broader agent. For patients experiencing side effects, dose reduction or a switch to an alternative with a different side‑effect profile often resolves the issue.
Frequently Asked Questions
Can I take Bactrim if I have a mild sulfa allergy?
Even a mild sulfa reaction can become severe when exposed to sulfamethoxazole. Most clinicians avoid Bactrim and pick an alternative like doxycycline or azithromycin.
Which alternative works best for uncomplicated cystitis?
Nitrofurantoin is usually first‑line because it concentrates in urine and has low resistance rates. If the patient can’t tolerate it, trimethoprim‑sulfamethoxazole (Bactrim) or a short course of fosfomycin are other options.
Is it safe to use azithromycin during pregnancy?
Azithromycin is classified as pregnancy category B, meaning animal studies showed no risk and there’s no evidence of harm in humans. Doctors often choose it when a macrolide is needed.
Why does ciprofloxacin cause tendon pain?
Fluoroquinolones interfere with collagen synthesis, weakening tendons-especially the Achilles. The risk rises with age, steroid use, or kidney disease, so clinicians limit use when possible.
What should I do if I develop a rash on Bactrim?
Stop the medication immediately and contact a healthcare provider. A rash could indicate a mild allergy or a serious skin reaction; prompt evaluation is essential.
Mithun Paul
Bactrim’s sulfonamide component raises valid concerns regarding renal function and hypersensitivity.
Sandy Martin
I’ve seen a lot of patients struggle with the photosensitivity side‑effect of Bactrim, especially during summer months.
While it’s an effective combo for many UTIs, clinicians should weigh kidney function carefully.
In my experience, a short course often suffices, reducing the risk of electrolyte disturbances.
For those with a known sulfa allergy, alternatives like nitrofurantoin or doxycycline are safer choices.
Always double‑check the dosage instructions; a simple mistake can lead to unnecessary side effects.
Steve Smilie
The pharmacodynamic synergy of sulfamethoxazole and trimethoprim epitomizes a classic “double‑hit” strategy, wherein successive inhibition of folate synthesis cascades precipitates bacterial demise.
Such a mechanism, while laudable, also imposes a metabolic burden on host nephron units, manifesting as heightened serum creatinine in susceptible cohorts.
Moreover, the specter of resistance looms ominously, particularly in regions plagued by rampant ESBL‑producing E. coli.
To circumvent these pitfalls, one might contemplate macrolide or fluoroquinolone alternatives, each possessing a distinct resistance tableau.
Nonetheless, the allure of a twice‑daily, broad‑spectrum regimen cannot be dismissed outright.
Clinicians must, therefore, calibrate therapy against individual comorbidities and local antibiograms.
In sum, Bactrim remains a formidable option, yet its application demands judicious clinical discernment.
Josie McManus
Totally get where you’re coming from – the kidney thing can be a real headache.
If you’re worried, swapping to nitrofurantoin for a simple cystitis is usually painless.
Just make sure the patient’s eGFR is above 60 before you do.
Heather Kennedy
From a pharmacokinetic standpoint, Bactrim achieves peak plasma concentrations within 1‑2 hours post‑dose, facilitating rapid eradication of susceptible pathogens.
However, its biotransformation via hepatic CYP2C9 can precipitate drug‑drug interactions, especially with anticoagulants.
Clinicians should monitor INR levels when co‑prescribing warfarin.
Alternative agents such as doxycycline, which bypass hepatic metabolism, may be preferable in polypharmacy scenarios.
Janice Rodrigiez
Nice summary – watch those INR spikes.
Roger Cardoso
One must consider that the pharmaceutical lobby has a vested interest in keeping Bactrim on the market, downplaying its nephrotoxic potential.
The data on long‑term renal outcomes is conveniently buried in paywalled journals.
Meanwhile, cheaper generics are pushed as first‑line, regardless of patient‑specific risks.
It's worth questioning whether the “broad‑spectrum” label is more marketing than science.
Alternative antibiotics with more transparent safety profiles should be evaluated.
Patients deserve full disclosure about possible tendon or kidney complications.
barry conpoes
Look, folks, Bactrim’s been a staple in American clinics for decades, and that’s for a reason.
We’ve got the data, the experience, and the supply chain to back it up.
If you’re chasing every conspiracy, you’ll miss the practical benefits.
Kristen Holcomb
Hey team, just a quick note – if you’re prescribing Bactrim to someone with a sulfa allergy, remember to double‑check the allergy list; we don’t want any unwanted rash.
Also, for pregnant patients, azithromycin is often a safer bet, especially in the second trimester.
Keep an eye on kidney function labs; a rise in creatinine could mean you need to switch drugs.
And don’t forget that nitrofurantoin is contraindicated if eGFR < 30.
Stay safe out there!
justin davis
Oh great, another post about Bactrim!!! Because we definitely need more “which antibiotic is best” debates!!!
Just take a deep breath, read the side‑effect list, and maybe-just maybe-ask a pharmacist!!!
Seriously, it’s not rocket science!!!
Choose wisely!!!
David Lance Saxon Jr.
In the grand tapestry of antimicrobial stewardship, the selection of Bactrim versus its rivals resembles a dialectical synthesis of efficacy and ethical responsibility.
The one must first acknowledge the Hegelian thesis: Bactrim offers a robust, dual‑mechanistic assault on bacterial folate pathways, thereby delivering commendable clinical outcomes.
The antithesis emerges in the form of its adverse effect profile-renal strain, photosensitivity, and the specter of sulfa hypersensitivity-casting doubt upon its universal applicability.
From a pharmaco‑ethical perspective, the practitioner is compelled to weigh the utilitarian benefit to the patient against the potential iatrogenic harm.
Moreover, the epidemiological data on regional resistance patterns functions as an ontological constraint, limiting the universal claim of Bactrim’s superiority.
When local E. coli isolates display escalating resistance, the synthesis leans toward alternative agents such as nitrofurantoin or a macrolide, thereby preserving therapeutic integrity.
Conversely, in settings where susceptibility remains high, the pragmatic choice may indeed be Bactrim, embodying the principle of “the right drug, right dose, right duration.”
Consider also the pharmacoeconomic dimension: generic Bactrim often presents a cost‑effective option, mitigating financial barriers to care.
Yet, cost should never eclipse patient‑centered values, especially in populations with known sulfa allergies or compromised renal function.
Thus, the clinician must engage in a phenomenological assessment, interrogating the patient’s comorbidities, concomitant medications, and lifestyle factors.
For example, a patient with a propensity for outdoor activities may suffer undue photosensitivity, prompting a shift toward doxycycline or azithromycin.
Similarly, the presence of G6PD deficiency contraindicates certain alternatives, further refining the decision tree.
In summation, the choice between Bactrim and its alternatives is not a binary dichotomy but a multidimensional algorithm, integrating microbiological data, patient physiology, ethical stewardship, and socioeconomic context.
Therefore, the astute prescriber navigates this complexity with both scientific rigor and compassionate insight.
Moore Lauren
Well put – choices are never that simple.
Jonathan Seanston
Hey everyone, just wanted to chime in and say that I’ve found the interactive selector tool quite handy for quick decisions.
Sukanya Borborah
Honestly, the tool feels like a half‑baked UI that throws a bunch of buzzwords at you without proper validation – the dropdowns are clunky and the CSS looks like it was scraped from a 2010 blog.
bruce hain
While Bactrim is efficacious, its sulfa component renders it unsuitable for patients with documented sulfonamide hypersensitivity.
Stu Davies
👍 Good reminder! 🙌
Nadia Stallaert
It is absolutely baffling, and I must emphasize, that the entire discourse surrounding antibiotic selection often devolves into a cacophony of half‑truths, misinterpreted data, and, dare I say, an almost conspiratorial denial of the very real risks posed by over‑prescription!!!
We are constantly bombarded with claims that Bactrim is “the silver bullet,” yet the literature is peppered with reports of renal impairment and severe cutaneous adverse reactions!!!
One cannot ignore the fact that pharmaceutical conglomerates have a vested interest in promoting broad‑spectrum agents, thereby ensuring market dominance!!!
Furthermore, the subtle influence of guideline committees, who may be swayed by industry funding, adds another layer of complexity to our decision‑making processes!!!
In the end, the prudent clinician must dissect each study, weigh the statistical significance, and consider patient‑specific variables before declaring any one drug the ultimate solution!!!
Therefore, let us approach antibiotic stewardship with a critical eye and an unwavering commitment to evidence‑based practice!!!
Greg RipKid
Totally agree – staying critical is key.
John Price Hannah
The tragedy of Bactrim’s side effects is a melodramatic saga that haunts the very soul of antimicrobial therapy!!! Its nephrotoxic whispers echo through the corridors of hospitals, while patients lament the blazing sun of photosensitivity!!! Yet, in the dark, it also shines as a heroic defender against stubborn pathogens, a duality that fuels endless debate!!!
Echo Rosales
Not every case needs a broad‑spectrum weapon; sometimes narrow‑targeted therapy is wiser.