Delayed Antibiotic Allergy: What It Is and How It Affects Your Treatment
When your body reacts to an antibiotic days after you start taking it, that’s a delayed antibiotic allergy, a type of immune response that doesn’t show up right away but can still be serious. Also known as late-onset drug hypersensitivity, it’s different from the quick, dramatic reactions people usually think of—like hives or swelling after the first dose. This one sneaks in: maybe a rash on day four, fever on day six, or swollen lymph nodes after a week. It’s often confused with a viral infection or even a side effect, which is why so many people keep taking the drug until it’s too late.
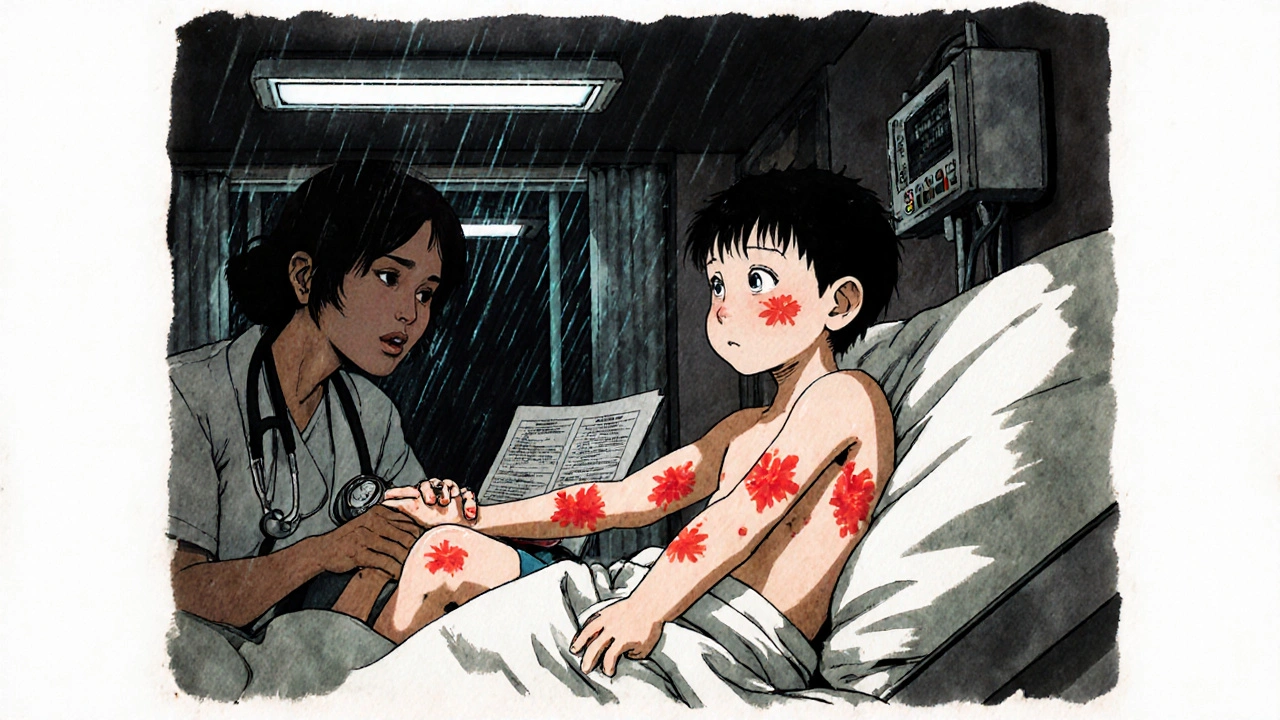
Most delayed antibiotic allergies, typically linked to beta-lactam antibiotics like penicillin and amoxicillin. Also known as T-cell mediated reactions, they happen because your immune system slowly recognizes the drug as a threat. Unlike immediate allergies that involve IgE antibodies, these involve T-cells that take time to activate. That’s why symptoms appear 48 to 72 hours—or even up to two weeks—after starting the medication. Common forms include maculopapular rashes, drug fever, and in rare cases, serious conditions like DRESS syndrome or Stevens-Johnson syndrome. The key is recognizing the pattern: if you got sick after starting an antibiotic and didn’t have symptoms before, it might not be the flu—it could be your body rejecting the drug.
This isn’t just about discomfort. A delayed antibiotic allergy, can lead to unnecessary hospital visits, wrong diagnoses, and even life-threatening complications if ignored. Also known as non-IgE mediated hypersensitivity, it’s often underdiagnosed because doctors don’t always test for it. Many patients are told they’re "just sensitive" or given another antibiotic without realizing the root cause. That’s dangerous—if you’ve had one delayed reaction, you’re at higher risk for another, even with different drugs in the same class. And if you’re labeled "allergic to penicillin" based on a delayed reaction, you might end up on broader-spectrum antibiotics that cost more, cause more side effects, and increase antibiotic resistance.
What you’ll find in the posts below are real-world cases and clear explanations of how these reactions show up, how they’re confused with other conditions, and what to do when you suspect one. You’ll see how antibiotics like Bactrim, tetracycline, and others can trigger these delayed responses—and why some kids and older adults are more vulnerable. There’s also guidance on how to track symptoms, what labs to ask for, and how to talk to your doctor about alternatives. No fluff. Just what you need to protect yourself when antibiotics are involved.
Serum Sickness-Like Reactions to Antibiotics: What Parents and Doctors Need to Know
Serum sickness-like reactions are delayed, non-allergic responses to antibiotics like cefaclor, often mistaken for true allergies. Learn the symptoms, how it's diagnosed, and why avoiding all penicillins is unnecessary.