Medication Side Effect Checker
How This Works
Based on medical guidelines from the FDA, CDC, and major health organizations.
Never stop taking medication without consulting your doctor.
This tool helps you understand symptoms better but is not medical advice.
People take medication to feel better. But too often, fear of side effects makes them quit-sometimes with dangerous results. You might think that if you feel nauseous after taking your pill, you should just stop. Or that if your infection feels better, you don’t need to finish the antibiotics. These ideas sound reasonable. They’re also wrong. And they’re costing lives.
Myth: If Side Effects Happen, Stop Taking the Medicine
It’s one of the most common reasons people quit their prescriptions. You take your blood pressure pill and get dizzy. You start an antibiotic and feel sick to your stomach. Your first thought? ‘This isn’t worth it.’ So you stop. But here’s the truth: most side effects aren’t dangerous-and they’re often manageable. The FDA reports that only 10-20% of patients experience any side effects at all. And of those, the majority can be fixed without quitting the drug. Nausea from antibiotics? Take them with food. Dizziness from blood pressure meds? Try taking them at night. A 2020 study found that simple timing changes reduced nausea by 68%. Stopping abruptly can make things worse. Antidepressants, for example, can cause withdrawal symptoms in over half of patients who quit cold turkey. Dizziness, ‘brain zaps,’ and insomnia aren’t signs the drug isn’t working-they’re signs your body is adjusting. A 2019 review found 56% of patients who stopped antidepressants suddenly experienced these effects. Heart patients are especially at risk. Nearly 3 in 10 stop beta-blockers after a heart attack because they feel tired or sluggish. But a 2022 study of over 14,000 patients showed those who quit had more than three times the risk of another heart attack.Myth: You Can Stop Antibiotics When You Feel Better
You’ve had a bad cough for days. You take your antibiotics for three days. You feel fine. So you toss the rest. You’re not alone. A 2022 survey found 63% of Americans believe it’s okay to stop antibiotics once symptoms fade. But here’s what you’re not hearing: feeling better doesn’t mean the infection is gone. Bacteria don’t follow your schedule. Even if you’re 90% better, there are still millions of bugs left. Stopping early lets the strongest ones survive-and they multiply. That’s how antibiotic resistance starts. The CDC says 2.8 million Americans get antibiotic-resistant infections every year. 35,000 die from them. A 2020 meta-analysis of 45 studies showed that skipping just one dose of antibiotics increases the chance of a resistant infection by 17%. The Infectious Diseases Society of America is clear: symptom relief is not the same as bacterial eradication. Most infections need 7 to 14 days to fully clear. Finishing the course isn’t about being obedient-it’s about survival.Myth: Statins Cause Severe Muscle Pain for Most People
Statins save lives. They lower cholesterol, prevent heart attacks, and reduce strokes. But many people quit them because they think statins cause muscle pain. One 2021 study found 74% of patients stopped statins within the first year. Here’s the reality: the science doesn’t back it up. The Cholesterol Treatment Trialists’ Collaboration analyzed data from 174,000 people across 27 trials. They found that statin users had only 0.9% more muscle symptoms than those on placebo. That’s less than 1 in 100. In a 2018 New England Journal of Medicine study, 90% of patients who believed they couldn’t tolerate statins were able to take them again-once they didn’t know whether they were getting the real drug or a sugar pill. The pain people feel? Often not from the statin. It’s from aging, inactivity, or other conditions. Hydrophilic statins like pravastatin and rosuvastatin are even safer-they penetrate muscle tissue 70% less than older types. If you’re worried, talk to your doctor about switching. Don’t quit.
Myth: OTC Pain Relievers Are Just as Good as Prescription Drugs
You’ve got chronic back pain. You reach for ibuprofen or acetaminophen. It helps a little. So you keep taking it. But OTC painkillers have hard limits. Ibuprofen maxes out at 1,200mg per day. Acetaminophen at 3,000mg. For moderate to severe pain, that’s not enough. A 2022 study found 68% of chronic pain patients get inadequate relief from OTC meds alone. Waiting to see a doctor costs time-and health. The American Academy of Pain Medicine says people delay professional care for an average of 14.7 months because they rely on OTC drugs. That delay makes pain worse, harder to treat, and more likely to become permanent. And OTC doesn’t mean harmless. Acetaminophen causes over 56,000 emergency room visits a year in the U.S. Liver damage can happen at doses over 4,000mg. Ibuprofen causes 10,000 hospitalizations annually from stomach bleeding. These aren’t rare accidents. They’re predictable results of long-term misuse.Myth: Prescription Drugs Are Safer Than Illicit Drugs
This one is deadly. People think because a doctor prescribed it, the drug is safe. That’s not true. Prescription opioids are the leading cause of opioid misuse in the U.S. The National Institute on Drug Abuse says 53% of new opioid cases in 2022 started with pills taken from a friend’s medicine cabinet. Prescription opioids carry a 23% risk of addiction after just 30 days. In 2022, they were involved in 18,000 overdose deaths. And mixing them with alcohol? That’s a recipe for disaster. A 2022 study found the risk of death jumps 47% when people combine prescription meds with alcohol. Acetaminophen and alcohol together cause 450 liver failure deaths each year. Illicit drugs like fentanyl are more dangerous per dose-but prescription drugs are more accessible. That’s why they’re the gateway. Never share your meds. Never take someone else’s. And never assume a pill is safe just because it came in a bottle.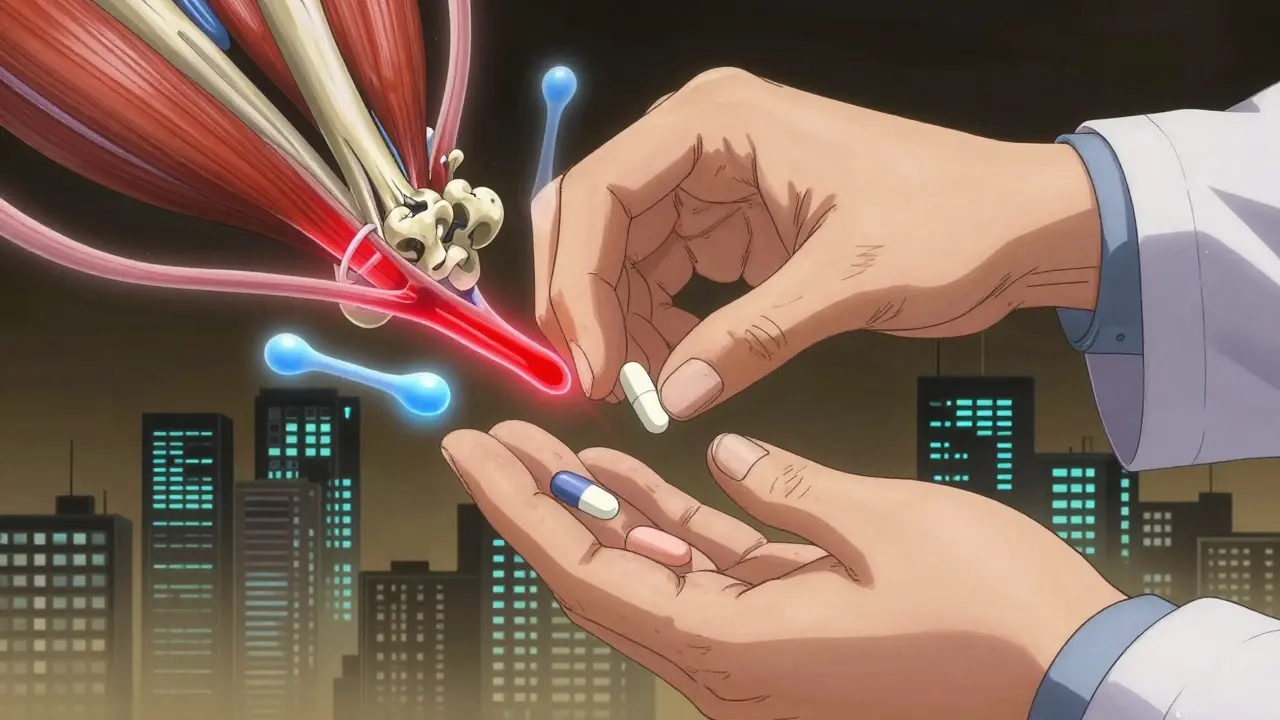
What You Can Do Instead
You don’t have to suffer through side effects. You don’t have to guess what’s normal. Here’s what works:- Call your doctor or pharmacist before stopping. Most side effects can be adjusted. A 2023 study found patients who used the ‘teach-back’ method-where they repeat instructions back to their provider-were 32% more likely to stick with their meds.
- Use adherence tools. Apps and smart pill bottles that remind you and track intake help you distinguish real side effects from normal symptoms. One study showed they cut unnecessary discontinuations by 39%.
- Ask about alternatives. If a drug isn’t working, there’s probably another option. For statins, switching from lipophilic to hydrophilic types reduces muscle pain. For antibiotics, timing and food make a big difference.
- Join a support group. Reddit’s r/Pharmacy and PatientsLikeMe have over 1.2 million users sharing real experiences. 63% of people who quit meds due to side effects were able to restart them after talking to a provider.
Final Thought: Your Medication Is a Team Effort
You’re not alone in this. Doctors, pharmacists, and nurses are trained to help you manage side effects-not just hand you a script and walk away. The American Pharmacists Association found that medication therapy management sessions reduced side effect-related stops by 41%. That’s not magic. It’s communication. Medication isn’t about fear. It’s about balance. The goal isn’t to feel zero side effects. It’s to feel better than you did before. And that only happens when you stick with the plan-and ask for help when you need it.Is it safe to stop my medication if I think the side effects are too much?
No. Stopping medication without talking to your doctor can lead to serious health risks, including withdrawal symptoms, worsening of your condition, or even life-threatening complications. Most side effects can be managed with adjustments like changing the time you take the pill, taking it with food, or switching to a different drug. Always consult your provider before making any changes.
Why do I feel worse after starting a new medication?
It’s common to feel off when starting a new drug. Your body is adjusting. Many side effects, like nausea, dizziness, or fatigue, fade within days or weeks. In some cases, what you’re feeling isn’t a side effect at all-it’s the ‘nocebo effect,’ where expecting discomfort causes real symptoms. Studies show up to 47% of reported side effects are linked to expectation, not the drug itself. Talk to your provider before assuming it’s the medication.
Can I skip doses of antibiotics if I feel better?
No. Stopping antibiotics early-even if you feel fine-allows surviving bacteria to become resistant. This leads to harder-to-treat infections in the future. The CDC and Infectious Diseases Society of America stress that symptom improvement doesn’t mean the infection is gone. Most infections require 7-14 days of treatment to kill nearly all bacteria. Always finish your full course.
Are statins really safe if they cause muscle pain?
Statins cause muscle pain in fewer than 1% of users. Most people who think they can’t tolerate statins can actually take them after switching to a different type, like pravastatin or rosuvastatin, which are less likely to affect muscles. In blinded studies, 90% of patients who believed they had statin-related pain could take the drug without issues. Muscle pain is often caused by other factors like aging or lack of activity. Don’t quit without testing it out with your doctor.
Can I take OTC painkillers long-term for chronic pain?
Long-term use of OTC pain relievers like ibuprofen or acetaminophen carries serious risks. Ibuprofen can cause internal bleeding, and acetaminophen can lead to liver failure-even at doses slightly above the recommended limit. For chronic pain, OTC drugs are rarely enough. Delaying proper treatment by relying on them can make your condition worse. Talk to a pain specialist instead.
Is it dangerous to take someone else’s prescription medication?
Yes. Prescription drugs are tailored to individual health conditions, weights, and other medications. Taking someone else’s pills can cause dangerous interactions, overdose, or addiction. In 2022, 30% of opioid overdose deaths involved medications not prescribed to the person. Never take a drug meant for someone else-even if it’s for the same symptom.
Ashley Porter
Let’s be real - most side effects are just your body throwing a tantrum because it’s not used to the new chemistry. The FDA data is solid: under 20% even report anything, and half of those are just temporary. I’ve been on three different SSRIs - each started with brain fog and nausea. Took me two weeks to realize I wasn’t dying, just adapting.
Pro tip: timing matters. Switching my fluoxetine from morning to bedtime killed the nausea. No magic, just pharmacokinetics.
Mohammed Rizvi
People treat antibiotics like a Netflix binge - watch the first three episodes, decide it’s ‘good enough,’ and quit. Meanwhile, the bacteria are throwing a victory party in your gut with a banner that says ‘Resistance Is Futile.’
2.8 million resistant infections a year? That’s not a statistic - that’s your cousin’s uncle’s friend who got sepsis because he stopped his pills when he ‘felt better.’
Nicholas Miter
Statins and muscle pain? I used to swear mine were from the drug. Turned out I was just sitting on my butt all day and blaming the pill. Switched to rosuvastatin, started walking 30 mins a day - pain vanished. Turns out, aging + inactivity = fake side effect.
Doctors aren’t trying to poison you. They’re trying to keep your heart from turning into a raisin.
TONY ADAMS
you ever just feel like your meds are making you a zombie? i stopped mine and now i feel like me again. who cares about the science if i feel better?
George Rahn
It is a profound societal failure that the populace has come to view pharmacological intervention as a form of moral weakness - as if the body’s natural equilibrium is somehow sacred, and modern medicine, an affront to Darwinian purity.
One cannot outwit evolution by ignoring evidence-based therapeutics. To cease antihypertensives because of transient vertigo is not autonomy - it is epistemic arrogance masquerading as self-determination.
Ashley Karanja
I’ve been on a beta-blocker since my MI and honestly, the fatigue was brutal at first. I thought I was just getting older - until I read that 30% of people quit and triple their risk of another event. That scared me into staying on it.
Then I started using a smart pill bottle with reminders and mood tracking - and realized my ‘fatigue’ was mostly sleep disruption from anxiety about the meds themselves. The nocebo effect is real, y’all.
I joined PatientsLikeMe and found 8 other people who had the exact same experience. We all switched to taking ours at night. Now I run 5Ks. I’m not ‘cured’ - I’m managed. And that’s enough.
Neil Thorogood
OTC painkillers are the new nicotine patches - everyone thinks they’re harmless because you can buy them next to gum and batteries.
Acetaminophen: liver failure. Ibuprofen: internal bleeding. And yet, people take them like candy for 14 months while their spine turns to dust.
Go see a pain specialist. Your body isn’t a DIY project.
Angie Thompson
My grandma took her statin for 12 years. Never had a problem. Then she heard a rumor on Facebook that they cause dementia. She stopped. Three months later - stroke.
Doctors don’t give out magic pills. They give out tools. And if you don’t use the tool, you can’t fix the problem. Don’t let TikTok be your pharmacist.
rasna saha
I used to stop antibiotics when I felt better too. Then I got a UTI that turned into sepsis. Took me three months to recover. Now I finish every course. Even if I feel fine on day three.
It’s not about being obedient. It’s about not ending up in ICU because you thought you knew better.
Geoff Miskinis
One must interrogate the epistemological foundations of the ‘teach-back’ method. Is it not merely a performative compliance mechanism designed to absolve clinicians of responsibility for patient education?
And yet - the 32% adherence increase is statistically significant. One wonders whether this is a triumph of behavioral psychology or a symptom of a broken healthcare system that requires patients to recite instructions like catechism to be deemed worthy of care.
Curtis Younker
Look - I get it. Pills are scary. But your body’s not your enemy. The real enemy is the myth that you’re supposed to feel perfect to be healthy.
Medication isn’t about zero side effects. It’s about feeling better than you did before you started.
My buddy quit his antidepressants because he ‘felt weird.’ He ended up in the ER. Now he’s back on them, plus therapy. He’s alive. That’s the win.
Shawn Raja
Someone said ‘never share meds’ - and I’m like… how is this still a thing in 2025?
People are handing out oxycodone like Halloween candy. ‘Oh, I got a script for back pain - you got a headache? Here.’
That’s not kindness. That’s a death sentence with a pharmacy label.