Hyperkalemia Risk Calculator
Assess Your Risk
This calculator estimates your risk of developing hyperkalemia (high potassium levels) when taking trimethoprim antibiotics based on key factors from medical studies.
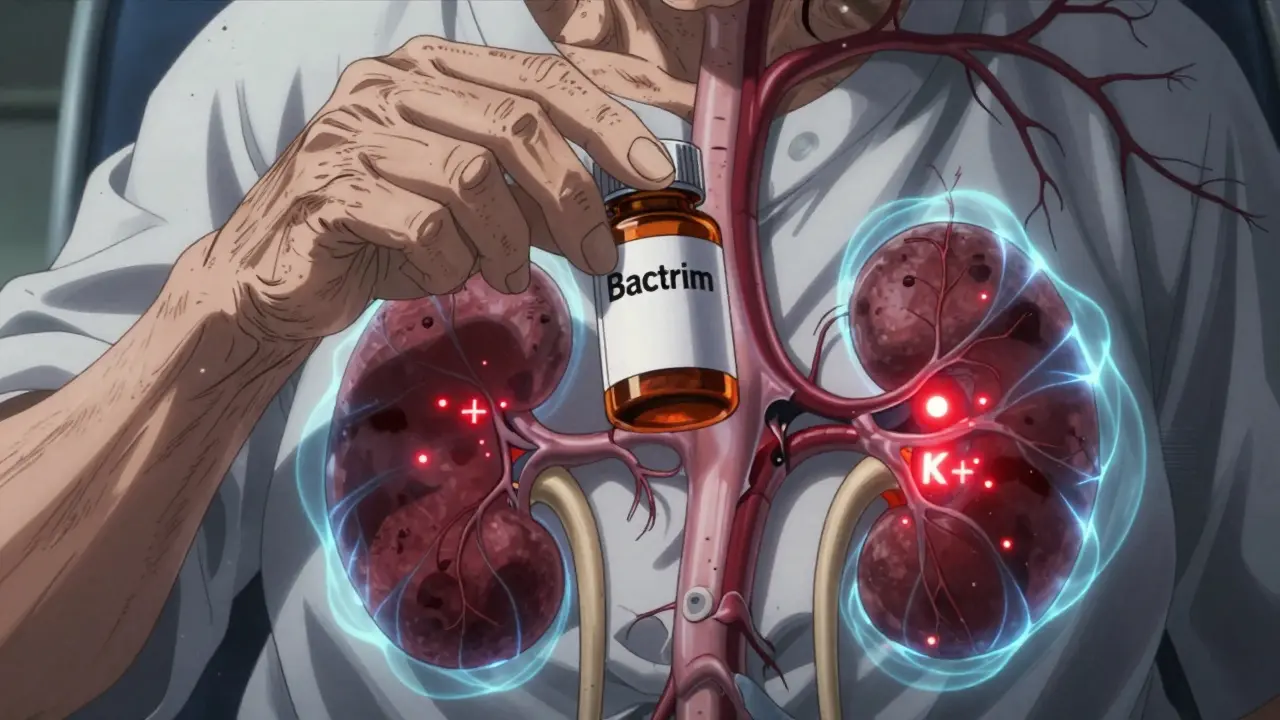
When you take an antibiotic like Bactrim or Septra for a urinary tract infection, you probably don’t think about your potassium levels. But for some people, this common drug can quietly push potassium into dangerous territory-fast. Trimethoprim, one half of the combo drug trimethoprim-sulfamethoxazole, doesn’t just kill bacteria. It also acts like a hidden diuretic that stops your kidneys from getting rid of potassium. And if you’re over 65, have kidney trouble, or take blood pressure meds like lisinopril or losartan, this isn’t just a minor concern. It can land you in the hospital-or worse.
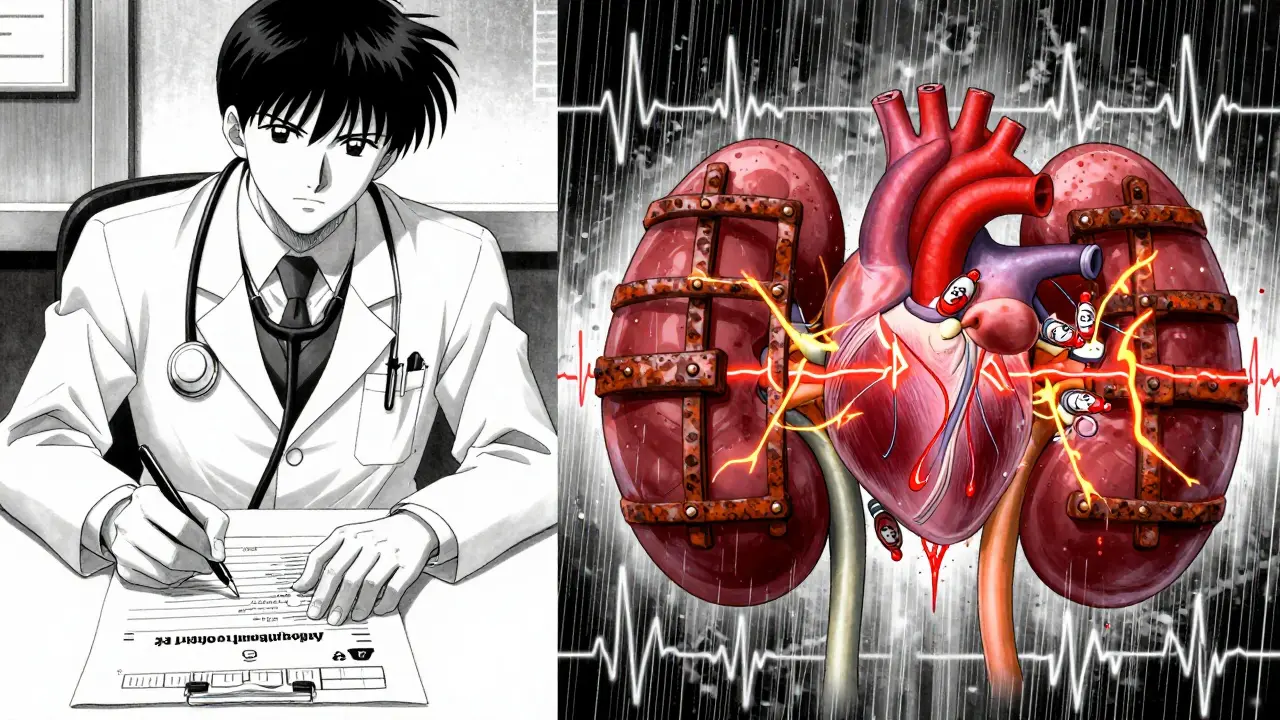
How Trimethoprim Tricks Your Kidneys
Trimethoprim looks a lot like a drug called amiloride, which is used to treat high blood pressure and heart failure. Both block tiny sodium channels in the kidney’s filtering units, called the distal convoluted tubule. When these channels shut down, sodium doesn’t get reabsorbed the way it should. That messes up the electrical signal your kidneys need to push potassium out into your urine. The result? Potassium builds up in your blood.
This isn’t slow or subtle. Studies show potassium levels can jump by 0.5 to 1.5 mmol/L within just 48 to 72 hours of starting trimethoprim. That might not sound like much, but when your normal range is 3.5 to 5.0 mmol/L, going from 5.1 to 6.8 is a medical emergency. High potassium can cause irregular heartbeats, muscle weakness, and even cardiac arrest.
What makes this worse is that trimethoprim concentrates in the kidneys at levels 10 to 50 times higher than in your bloodstream. So even if your blood test looks normal, your kidneys are getting a heavy dose. That’s why even low-dose, short-term use-like a 3-day course for a UTI-can trigger problems in vulnerable people.
Who’s at the Highest Risk?
Not everyone who takes trimethoprim gets high potassium. But certain groups are in the danger zone:
- People over 65
- Those with chronic kidney disease (eGFR under 60)
- Patients taking ACE inhibitors (like enalapril) or ARBs (like valsartan)
- People already on potassium-sparing diuretics (like spironolactone)
- Those with diabetes or heart failure
A 2014 study in JAMA Internal Medicine found that older adults on ACE inhibitors or ARBs who took trimethoprim had a 6.7-fold higher risk of being hospitalized for high potassium than those who took amoxicillin. That’s not a small increase. It’s a massive red flag.
And here’s the kicker: you don’t even need to have bad kidneys to be at risk. A 2023 case report described an 80-year-old woman with normal kidney function (creatinine 0.7 mg/dL) who developed a potassium level of 7.8 mmol/L-deadly territory-just 72 hours after starting a single daily dose of Bactrim for pneumonia prevention. She had no prior history of high potassium. One pill, three days, cardiac arrest.
How Common Is This?
It’s more common than most doctors realize. In healthy adults, about 1.2% of people on other antibiotics develop high potassium. But with trimethoprim? That number jumps to 8.4%. For patients with kidney disease, it’s nearly 1 in 6-17.6%.
And it’s not just a few isolated cases. Between 2010 and 2020, the FDA’s adverse event database recorded over 1,200 cases of trimethoprim-related hyperkalemia, including 43 deaths. Nearly 70% of those deaths happened in people over 65. In one Reddit thread, a doctor wrote about a 72-year-old woman on lisinopril who hit a potassium level of 6.8 after three days of Bactrim. She needed emergency dialysis.
Meanwhile, a 2022 analysis showed that nearly 30% of all trimethoprim prescriptions in the U.S. go to people over 65. That’s over 4 million prescriptions a year to a group that’s three times more likely to have dangerous reactions.
Why Do Doctors Still Prescribe It?
Because it works. Trimethoprim-sulfamethoxazole is cheap, effective, and great for treating urinary tract infections, sinus infections, and even preventing pneumonia in people with weakened immune systems. For someone with HIV or who’s had an organ transplant, it’s often the best choice.
But here’s the problem: many doctors don’t check potassium before prescribing it. A 2023 survey found that only 41.7% of primary care doctors routinely test potassium levels before giving trimethoprim to patients on blood pressure meds. Emergency room doctors? Only 32.4% do it. Nephrologists? Almost all of them. But the people most likely to prescribe it-family doctors and ER docs-are the least likely to check.
That’s why some hospitals now have electronic alerts that pop up when a doctor tries to order Bactrim for someone on an ACE inhibitor. One study showed these alerts cut hyperkalemia cases by over half.

What Should You Do?
If you’re prescribed trimethoprim, here’s what you need to know:
- Ask if you’re at risk. Are you over 65? Do you take lisinopril, losartan, or similar meds? Do you have kidney disease or diabetes? If yes, ask if there’s a safer alternative.
- Get a baseline potassium test. Even if you feel fine, a simple blood test before you start the antibiotic can give you a reference point.
- Get tested again in 48 to 72 hours. That’s when potassium levels peak. Don’t wait until you feel weak or dizzy.
- Know the warning signs. Muscle cramps, fatigue, irregular heartbeat, nausea, or a strange fluttering in your chest? Call your doctor immediately.
- Don’t stop the drug on your own. If potassium is high, your doctor may tell you to stop trimethoprim and give you meds like calcium gluconate or insulin to lower it fast. In severe cases, dialysis is needed.
There are alternatives. For urinary tract infections, nitrofurantoin is just as effective and doesn’t raise potassium. For pneumonia prevention in immunocompromised patients, dapsone or atovaquone are options. Talk to your doctor about what’s right for you.
The Bottom Line
Trimethoprim isn’t evil. It saves lives. But it’s not harmless, either. It’s a drug that hides its danger. You can’t see it. You can’t feel it until it’s too late. That’s why awareness matters. If you’re taking blood pressure meds or have kidney issues, don’t assume your doctor knows the risk. Ask. Push. Get tested. A simple blood test before you start a 3-day course could prevent a life-threatening emergency.
For healthy people under 65 with no kidney problems or heart meds, the risk is low. But for millions of older adults on common prescriptions, this isn’t a theoretical concern. It’s a ticking clock-and it’s silent until it goes off.
Caitlin Foster
So let me get this right: a $5 antibiotic can quietly murder you if you're over 65 and take blood pressure meds?? And doctors are just... shrugging?? 🤯 I mean, I get it's cheap and effective-but if it's got a 1 in 6 chance of turning your heart into a malfunctioning microwave, why isn't this screaming from every pharmacy counter?? #StopTheSilentKillers
Andrew Gurung
Ah yes, the classic 'drug company hiding dangers' narrative. 😒 Meanwhile, real doctors are trying to treat UTIs in 80-year-olds with limited options. Nitrofurantoin? Great for bladder infections, useless for pneumonia. Dapsone? Causes hemolysis in G6PD-deficient patients (which is COMMON in certain populations). Atovaquone? $1,200 per course. So yes, trimethoprim is the *least worst* option-until you forget to check potassium. It's not the drug's fault-it's the lazy prescribing. 🤷♂️
Janice Holmes
I work in cardiology. Last month, a 73-year-old woman came in with ventricular tachycardia. Potassium: 7.2. She’d been on lisinopril for 12 years. Took Bactrim for a ‘sinus infection’-which was just allergies. No labs. No follow-up. She coded on the floor. We saved her. But she’s on dialysis now. This isn’t hypothetical. It’s Tuesday.
Alex Lopez
I'm a pharmacist. Every time I see trimethoprim prescribed to someone on an ARB, I flag it. 80% of the time, the prescriber says, 'Oh, I didn't know.' 15% say, 'I checked her labs last week.' 5% say, 'I don't care.' The system is broken. But here's the fix: EHR alerts. They work. Hospitals that implemented them cut hyperkalemia by 58%. So why aren't ALL hospitals doing this? Because bureaucracy > patient safety. 💉
Paula Alencar
Let us not forget: this is not an isolated phenomenon. It is a systemic failure of medical education, clinical decision support, and prescriber accountability. The fact that 32.4% of ER physicians do not routinely check potassium before prescribing trimethoprim-despite the FDA's 1,200+ adverse event reports-is not negligence. It is institutionalized ignorance. We must demand mandatory clinical decision support at the point of prescribing. Not as a suggestion. Not as an option. As a requirement. Lives are not data points. They are people. And people deserve better than this.
James Bowers
The data is clear. The risk is quantifiable. The consequences are fatal. Yet, we continue to allow low-risk, high-impact drugs to be prescribed without basic safeguards. This is not a matter of opinion. It is a matter of clinical protocol. If your hospital does not have an alert for trimethoprim + ACEi/ARB, you are not practicing medicine-you are gambling with human lives.
Satyakki Bhattacharjee
In my village, we use neem leaves for infections. No blood tests. No pills. No hospital. Why do we need this fancy science when nature gave us everything? This drug is not the problem. Our trust in machines is.
Olivia Goolsby
This is all a lie. The FDA doesn’t want you to know: potassium is a government tool to control the elderly. They push these drugs to make seniors dependent on dialysis so they can sell more machines. The ‘risk’ is manufactured. Why do you think they never mention that 90% of people who get hyperkalemia from Bactrim also had high-sodium diets? Coincidence? Or controlled exposure? 🤔 #BigPharmaLies #PotassiumControl
Chris Garcia
In Nigeria, we call this ‘the silent thief of breath.’ A man takes his medicine for blood pressure, then a fever, then a pill from the chemist-and one morning, he does not wake. No scream. No struggle. Just stillness. We do not have labs. We do not have alerts. We have prayers. And yet, this article-this careful, clinical truth-is a gift. It is the first time a Western voice has said: ‘This is not normal. This is not okay.’ Thank you.
Kishor Raibole
The statistical correlation between trimethoprim use and hyperkalemia is undeniably significant, as evidenced by the JAMA Internal Medicine study cited. However, one must exercise caution in extrapolating population-level data to individual clinical decision-making. The risk-benefit calculus must be evaluated within the context of antimicrobial stewardship, patient-specific comorbidities, and the absence of equally efficacious alternatives in certain clinical scenarios. To suggest that this agent should be universally avoided is to ignore the nuanced nature of clinical medicine.
Gerald Tardif
I’ve seen this play out twice in my clinic. One guy, 78, on losartan, took Bactrim for a UTI. Three days later, he couldn’t lift his arm. We caught it. He’s fine now. But here’s the thing: he didn’t know to ask. Neither did his doctor. So I started handing out one-pager sheets with the top 5 red flags. Now, 80% of my older patients bring them in before they pick up the script. Small change. Big impact. You don’t need a revolution. You just need to speak up.
Monika Naumann
This is why Western medicine is collapsing. You fear a pill that saves lives, while ignoring the real enemy: poor hygiene, bad diet, and lack of discipline. In India, we treat infections with fasting, turmeric, and discipline. We do not need your lab tests. We do not need your alerts. We need character. This article is weakness dressed as wisdom.