For millions of people around the world, taking a statin every day is just part of life-like brushing your teeth or drinking water in the morning. But for others, that same pill brings aching legs, tired muscles, or the fear that the cure might be worse than the disease. If you’ve been prescribed a statin, or are thinking about it, you’re probably wondering: Is this drug really helping me, or is it just making me feel worse?
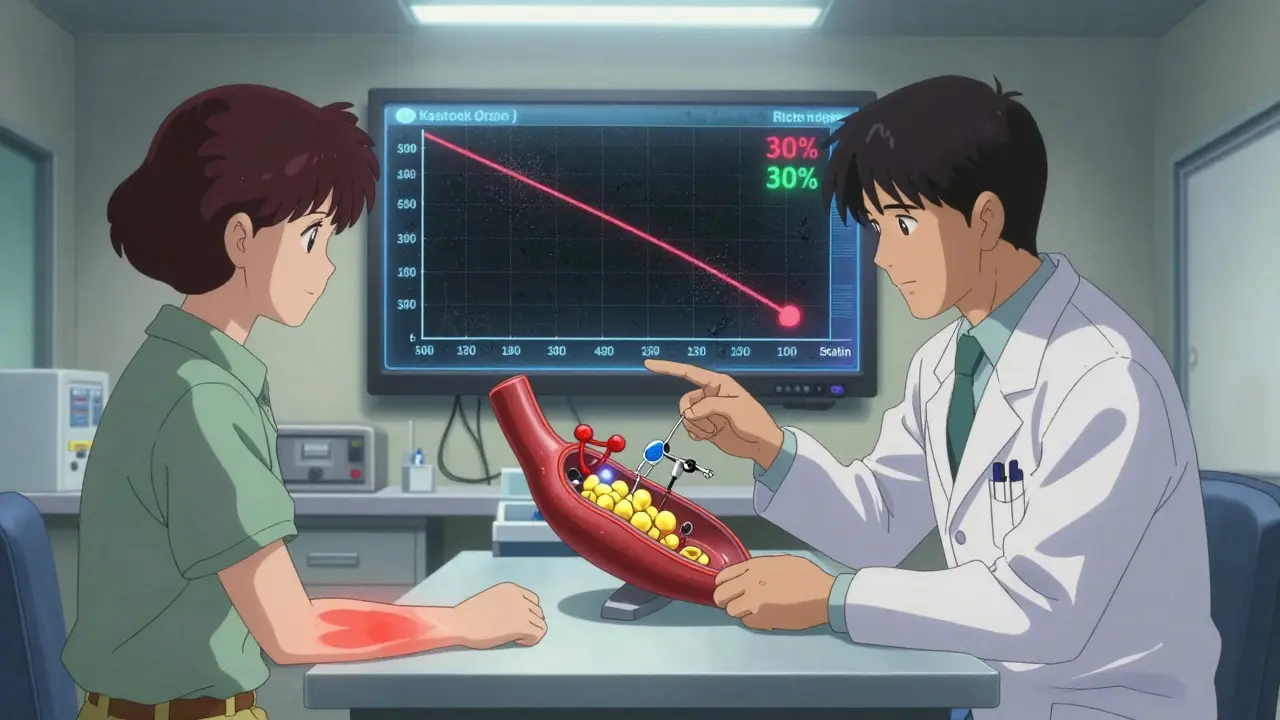
How Statins Actually Work
Statins don’t just lower cholesterol-they change how your body handles it. These drugs block a liver enzyme called HMG-CoA reductase, which is responsible for making cholesterol. When that enzyme slows down, your liver starts pulling more LDL (bad) cholesterol out of your bloodstream to use for itself. That’s why your blood test numbers drop. On average, statins cut LDL by about 70 mg/dL (1.8 mmol/L). That might not sound like much, but it translates to a 60% lower chance of having a heart attack or dying from heart disease.
It’s not just about cholesterol. Statins also reduce inflammation in your arteries, stabilize plaque so it doesn’t rupture, and improve how well the lining of your blood vessels works. Studies show these effects happen even before LDL levels drop significantly. That’s why someone with normal cholesterol but high inflammation can still benefit. A 2023 Stanford study found that statins help protect the cells lining your blood vessels-something that’s just as important as lowering numbers on a lab report.
Who Benefits the Most?
Not everyone needs a statin. The biggest winners are people who’ve already had a heart attack, stroke, or bypass surgery. For them, statins cut the risk of another event by about one-third. People with diabetes, especially if they’re over 40, also get strong protection. If you have high LDL (above 190 mg/dL) or a family history of early heart disease, statins can be a game-changer.
But here’s the catch: if you’re healthy, with no heart disease, no diabetes, and only mildly elevated cholesterol, the benefit is much smaller. For every 100 people like that, only about 1 or 2 might avoid a heart attack over five years. That’s why doctors now focus on overall risk-not just one number. Tools like the ACC/AHA risk calculator look at age, blood pressure, smoking, and family history to decide if statins make sense.
The Muscle Pain Problem
Let’s be honest: muscle pain is the reason most people stop taking statins. It’s not rare. Around 5% to 10% of users report aches, stiffness, or cramps-usually in the shoulders, thighs, or calves. For some, it’s mild and goes away after a few weeks. For others, it’s bad enough to quit.
The scary part? Only 0.1% of users develop rhabdomyolysis-a rare but dangerous condition where muscle tissue breaks down and can damage the kidneys. But that tiny number doesn’t help if you’re the one in 1,000. What matters more is how often people feel bad and don’t tell their doctor. Many assume it’s just aging, or that they’re out of shape. But if the pain started after you began the statin, it’s worth talking about.
Not all statins are the same. Simvastatin and atorvastatin are more likely to cause muscle issues than pravastatin or fluvastatin. Rosuvastatin can be tough on some people too, especially at higher doses. Switching statins is one of the first things doctors try when muscle pain shows up. Many patients find relief just by changing brands.
What to Do If You Have Muscle Pain
If you’re experiencing muscle discomfort, don’t just quit. Talk to your doctor. Here’s what usually happens:
- Your doctor checks your creatine kinase (CK) levels-a blood marker for muscle damage. If it’s normal, you likely have myalgia (pain without damage), not rhabdomyolysis.
- They may lower your dose. Sometimes, half a tablet still gives you 80% of the benefit with far less pain.
- They might switch you to a different statin. Pravastatin and fluvastatin are often better tolerated.
- Some people try coenzyme Q10 supplements. The science isn’t solid, but if it helps you feel better, it’s worth a trial under medical supervision.
- Exercise habits matter. Intense workouts while on statins can make muscle pain worse. Light walking or swimming is usually fine.
One patient I spoke with in Adelaide-let’s call her Lisa-had terrible leg cramps on rosuvastatin. She stopped cold turkey, and her cholesterol jumped back up. Her doctor switched her to low-dose pravastatin, and within three weeks, the cramps vanished. Her LDL stayed under 100. She’s been on it for two years now, no issues.
Why People Quit-and Why They Shouldn’t
Studies show nearly half of people stop taking statins within a year. The main reason? Side effects they think are real. But here’s the twist: in placebo-controlled trials, up to 70% of people who say they had muscle pain on statins had the same pain when they took a sugar pill. That doesn’t mean the pain isn’t real-it means your brain can trick you into blaming the pill.
Still, if you genuinely feel worse, your concerns are valid. The key is working with your doctor to find a solution, not giving up. Stopping statins means losing protection. A 2014 JAMA study found that people who quit had a 40% higher chance of having a heart attack in the next year. That’s not a risk worth taking unless you’ve found a safer alternative.

Alternatives and What’s Next
If statins don’t work for you, there are other options. Ezetimibe lowers cholesterol by blocking absorption in the gut. PCSK9 inhibitors are injectable drugs that drop LDL by 60% or more. They’re expensive but very effective for people who can’t tolerate statins.
Future treatments may be smarter. Researchers are working on statin-like drugs that target only the blood vessel benefits-without touching muscle cells. Stanford scientists are already testing versions that don’t interfere with the same pathways linked to muscle pain. It’s early, but the hope is clear: a statin that protects your heart without hurting your legs.
Final Thoughts
Statins are one of the most studied drugs in medical history. Their benefits for high-risk people are undeniable. But they’re not magic. They’re tools. And like any tool, they work best when used the right way.
If you’re at high risk for heart disease, the odds are strongly in favor of taking one. If you’re low risk and feeling awful, don’t accept muscle pain as normal. Ask your doctor: Is there a different statin? A lower dose? A different approach?
There’s no one-size-fits-all answer. But there is a path forward-for everyone who’s willing to keep talking, keep trying, and keep protecting their heart.
Do statins really prevent heart attacks?
Yes, for people at high risk. Large studies show statins reduce heart attacks by about 30% and strokes by 17% over five years. The benefit is strongest if you’ve already had a heart event, have diabetes, or have very high LDL. For low-risk people, the benefit is smaller but still present.
Is muscle pain from statins real or just in my head?
The pain is real. But not all muscle aches are caused by statins. In clinical trials, about 70% of people who reported muscle pain while on statins had the same symptoms when taking a placebo. That doesn’t mean it’s imaginary-it means other factors like aging, activity level, or other medications can contribute. The key is to work with your doctor to figure out if the statin is the main trigger.
Can I take a lower dose and still be protected?
Often, yes. Many people get 80% of the cholesterol-lowering benefit from half the standard dose. Lower doses also mean fewer side effects. If you’re on a high dose and having muscle pain, ask your doctor about switching to a lower dose or a different statin. You might not need to stop entirely.
Are generic statins as good as brand names?
Yes. Generic atorvastatin, simvastatin, and rosuvastatin are bioequivalent to their brand-name versions. They work the same way, have the same side effect profile, and are much cheaper-sometimes as low as $4 a month. There’s no reason to pay more unless your doctor has a specific reason to choose a brand.
Should I take CoQ10 with my statin?
The evidence is mixed. Statins lower CoQ10 levels in the body, and some people feel better taking supplements. But large studies haven’t proven it prevents muscle pain. Still, if you’re experiencing discomfort and your doctor agrees, trying CoQ10 for a few weeks is low-risk and might help. It’s not a cure, but it’s worth a trial.
Ken Cooper
I took atorvastatin for 3 years and honestly? My legs felt like lead pipes. I thought it was just getting old, but then I switched to pravastatin at half dose and boom-no more cramps. My doc said I got 80% of the benefit with 20% of the pain. That’s a win in my book. Also, generics are literally the same. No need to pay extra for fancy packaging.
Karianne Jackson
I quit statins after my thighs turned into concrete. My doctor said I was fine, but I felt like I was dying. Now I eat avocado every day and walk 10k steps. My cholesterol? Still high. But at least I can climb stairs without groaning.
Chelsea Cook
Oh honey, you think muscle pain is bad? Try explaining to your insurance company why you 'chose' to not take a $4 pill that 'saves lives' while you're on your third knee replacement. Statins are the OG wellness hack. If you can't handle a little soreness, maybe you should’ve skipped the donuts in the first place.
Alex Ogle
I’ve been on statins since I was 42. I’m 58 now. No heart issues. No muscle pain. Just a quiet life. But I’ve watched friends drop them because of 'side effects'-and then end up in the ER six months later. The science is solid. The fear? Often louder than the facts. That 70% placebo pain thing? It’s wild. Your brain will blame the pill even when it’s your couch, your coffee, or your dog barking too loud. Don’t let noise drown out data.
Jacob den Hollander
I’m a nurse in rural Kansas. I see this all the time. People stop statins because they read a blog that says 'cholesterol is a lie.' Then they come in with chest pain and a CK level of 8000. I get it-you’re scared. But your doctor isn’t trying to sell you something. They’re trying to keep you alive. If you’re in pain, say so. Try a different statin. Lower the dose. Take CoQ10. But don’t just quit. Talk. We’re here. We’ve seen this movie before. And the ending where you stop the pill? It’s never good.
John McDonald
I was skeptical too. Then I got my numbers checked after 6 months on low-dose rosuvastatin. LDL dropped from 180 to 85. I felt better. No pain. Just energy. I started biking again. My wife said I stopped grumbling. Statins aren’t magic. But they’re not poison either. It’s about balance. And listening. And not letting fear decide for you.
Chima Ifeanyi
The data is statistically significant but clinically marginal for low-risk populations. The NNT for primary prevention is approximately 100 over five years. Meanwhile, the number needed to harm for myalgia is 10-20. Ergo, the risk-benefit ratio is inverted for asymptomatic individuals with borderline hyperlipidemia. You’re conflating correlation with causation. Also, the ACC/AHA calculator is proprietary and overfits. It’s not evidence-it’s algorithmic bias dressed in white coats.
Andy Cortez
Statins? More like statin-SCAM. Big Pharma’s got us hooked on pills because they don’t want us to eat real food. Who invented cholesterol anyway? A guy in a lab coat with a clipboard and a smirk. My grandma ate bacon every day and lived to 94. You think your blood test matters more than her wisdom? Wake up. And CoQ10? That’s the real deal. The truth is buried under 2000 pages of FDA paperwork. Read the studies. Not the summaries.
Tori Thenazi
I know what they don’t tell you. Statins are linked to Alzheimer’s. And liver cancer. And depression. And they’re in the water supply now. I read a whistleblower report. It was redacted. But I have screenshots. My cousin’s neighbor’s sister took statins and her hair turned green. Not kidding. Google 'statin side effects whistleblower 2022'. I’ll wait. Also, your doctor gets kickbacks. Always.
Monica Warnick
I tried simvastatin. Felt like a zombie. Took CoQ10. Nothing. Switched to pravastatin. Still tired. Then I read that statins deplete mitochondrial energy. So I stopped. Now I take magnesium, walk barefoot on grass, and say affirmations. My LDL is 170. But I feel free. And isn’t that worth more than a number?
Tatiana Barbosa
I’ve been on a low dose for 8 years. No pain. No issues. My mom had a stent at 62. She quit statins because she 'felt weird.' Three months later, she had a stroke. Don’t be her. Talk to your doc. Try a switch. Lower the dose. But don’t ghost your heart. It’s been loyal. Give it a fighting chance.
Tom Forwood
I’m from the Midwest. We don’t do fancy meds. We do grit. I had a statin-induced muscle ache so bad I couldn’t open a jar. Went to my doc. Switched to fluvastatin. 20mg. Gone in 10 days. My cholesterol? Still down. My life? Still mine. You don’t need to suffer to survive. There’s always a way. Just ask. And don’t let fear make the call.
Andrew Jackson
The medical establishment has weaponized fear to sell pharmaceuticals. The lipid hypothesis is a flawed paradigm, rooted in 1950s corporate funding. The Framingham study was manipulated. Statins do not prevent heart disease-they mask symptoms while eroding cellular integrity. You are not a number. You are not a risk calculator. You are a human being. Reject the dogma. Seek truth. Reject the pill. Embrace nature. Sovereignty over submission.
Randy Harkins
I was scared too. But I talked to my doctor. We tried lower dose + CoQ10. It worked. I’m still here. My kids still have a dad. I don’t care if it’s placebo or science-I care that I feel okay. 🙏❤️ You’re not alone. There’s a path. Just don’t give up before you find it.
Ashlyn Ellison
Switched from rosuvastatin to pravastatin. Pain gone in two weeks. LDL stayed under 100. Done.