If you’re taking St. John’s Wort for mild depression, you might feel like you’ve found a natural solution that works without the side effects of prescription pills. But here’s the hard truth: St. John’s Wort doesn’t just sit quietly in your system-it actively changes how your body handles almost every major prescription drug you could be taking. And that’s not a small risk. It’s the kind of risk that can make your birth control fail, your transplant medication stop working, or your antidepressant turn dangerous.
How St. John’s Wort Changes Your Body’s Chemistry
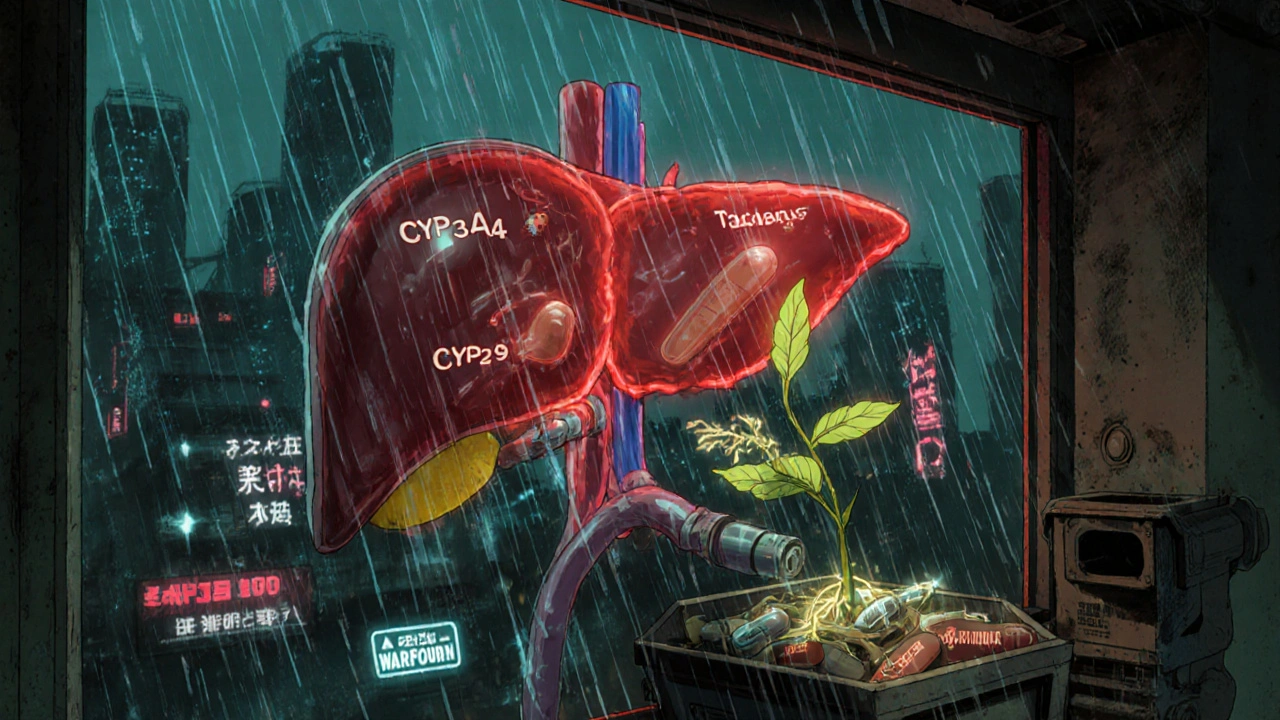
St. John’s Wort isn’t just a plant extract. It’s a powerful biological switch. The key player is hyperforin, a compound found in the herb that turns on a receptor in your liver called PXR. When this receptor flips on, your body starts producing more of certain enzymes-mainly CYP3A4, CYP2C9, and CYP1A2-that break down drugs. It also ramps up P-glycoprotein, a protein that pushes drugs out of your cells. Think of it like your liver suddenly getting a speed boost and flushing out medications before they can do their job.
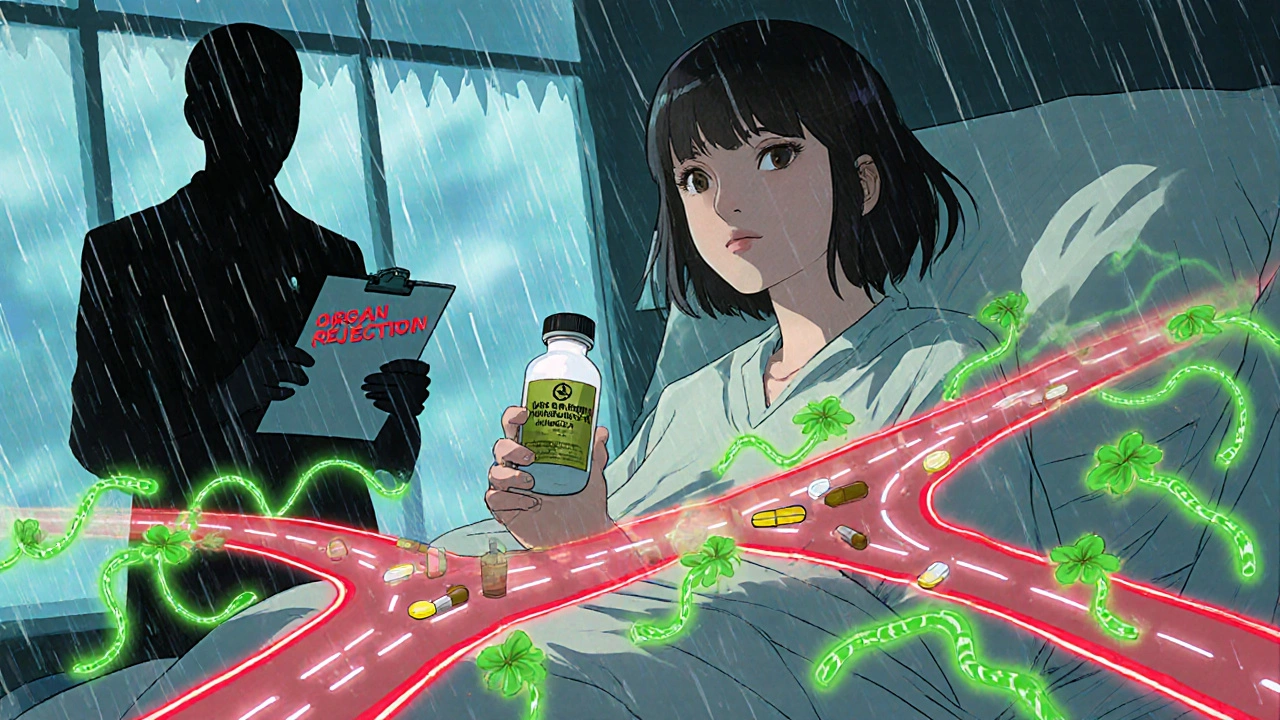
This isn’t theoretical. In 2019, a 34-year-old woman in the U.S. had a kidney transplant and was taking tacrolimus to stop rejection. Her levels were stable. Then she started taking St. John’s Wort. Eight weeks later, her tacrolimus levels dropped below the safety threshold. Her body rejected the kidney. She needed another transplant. That’s not a rare case. It’s one of dozens documented in medical journals.
The 12 Medication Categories That Can Fail With St. John’s Wort
St. John’s Wort doesn’t just interfere with one or two drugs. It messes with at least 12 major classes of prescriptions. Here’s what you need to watch out for:
- Immunosuppressants like cyclosporine, tacrolimus, and sirolimus-used after organ transplants. Even small drops in these levels can cause organ rejection.
- Anticoagulants like warfarin. One patient’s INR (a measure of blood clotting) dropped from 2.5 to 1.4 in just 10 days after starting St. John’s Wort. That’s a major spike in clotting risk.
- Oral contraceptives. There are documented cases of women getting pregnant while on the pill and taking St. John’s Wort. The herb lowers estrogen levels enough to make birth control ineffective.
- Antidepressants like SSRIs (Prozac, Zoloft) and SNRIs (Effexor). Combining them with St. John’s Wort can cause serotonin syndrome-a dangerous spike in serotonin that leads to high fever, seizures, and even death.
- HIV medications like protease inhibitors and non-nucleoside reverse transcriptase inhibitors. St. John’s Wort can slash their levels by up to 60%, making HIV treatment useless and increasing drug resistance.
- Heart medications like digoxin and some statins. Lowered levels mean uncontrolled heart rhythm or cholesterol.
- Chemotherapy drugs like irinotecan. Reduced effectiveness can mean cancer progression.
- Pain meds like oxycodone, methadone, and tramadol. St. John’s Wort can make them stop working, leaving patients in severe pain.
- Antifungals like itraconazole. These drugs are already tricky to dose. St. John’s Wort makes them even more unpredictable.
- Thyroid meds like levothyroxine. Patients have reported fatigue and weight gain after starting St. John’s Wort, likely due to reduced absorption.
- Antiepileptics like carbamazepine. Reduced levels can trigger seizures.
- Antivirals for hepatitis C and other chronic infections. These drugs have narrow therapeutic windows. St. John’s Wort can push them out of the safe range.
That’s not a list of possibilities. That’s a list of documented, life-threatening failures. The European Medicines Agency says St. John’s Wort shouldn’t be used with any drug that has a narrow therapeutic index-that means the difference between a helpful dose and a toxic one is tiny. Many of the drugs above fall into that category.
Why People Think It’s Safe-And Why They’re Wrong
Many people assume herbal means harmless. But St. John’s Wort is one of the most studied herbal supplements when it comes to drug interactions. In fact, it has over 50 documented interactions-far more than SAM-e or 5-HTP, which are also used for mood. Dr. David A. Flockhart, a leading pharmacologist, called it “the single most important herbal supplement in terms of drug interactions.”
And it’s not just the dose. A typical St. John’s Wort supplement contains 300-900 mg daily, standardized to 0.3% hypericin and 2-5% hyperforin. The hyperforin content is what drives the enzyme induction. Even a single 300 mg capsule can start changing your body’s drug metabolism within days. It takes about 10 days to reach full effect-and the changes can last for two weeks after you stop taking it. That’s why some people don’t realize what’s happening until weeks later, when their blood pressure spikes or their antidepressant stops working.
What Happens When You Mix It With Antidepressants
It’s ironic. People take St. John’s Wort because they want to avoid the side effects of SSRIs. But combining the two can trigger serotonin syndrome. Symptoms include agitation, confusion, rapid heart rate, sweating, shivering, muscle rigidity, and in severe cases, seizures, high fever, and unconsciousness. The Mayo Clinic warns this can be fatal.
One study in the Journal of Clinical Psychiatry followed 22 patients who took St. John’s Wort along with an SSRI. Four developed clear signs of serotonin syndrome. Three needed hospitalization. None of them knew the risk. They assumed “natural” meant “safe together.”
Even if you’re not on an SSRI, St. John’s Wort itself affects serotonin. It’s not just an herbal placebo. It has pharmacological activity. That’s why it works for mild depression-but also why it’s so dangerous when layered with other drugs.
Who Uses It-and Why It’s Still on Shelves
St. John’s Wort is still popular. In Germany, it’s used in about 20% of all depression treatments. In the U.S., about 4.7% of adults take it, mostly women aged 35-54. Sales peaked in 2000 at over $1 billion globally. Now, they’re down 37%-because more people are learning the risks.
But here’s the problem: in the U.S., the FDA doesn’t require pre-market approval for supplements. That means St. John’s Wort can be sold without proving safety or interaction warnings. Many bottles have tiny disclaimers on the back. Others say nothing at all. A 2023 FDA advisory specifically called St. John’s Wort a “high-risk supplement for drug interactions.” Yet you can still buy it next to the vitamins at your local pharmacy.
Compare that to Europe. Since 2004, the European Medicines Agency has required St. John’s Wort products to carry bold warnings about interactions with birth control, transplant drugs, and anticoagulants. In the U.S., that level of clarity is rare.
What to Do Instead
If you’re considering St. John’s Wort for depression, here’s what you need to do before even opening a bottle:
- Review every medication you take-including over-the-counter drugs, heartburn pills, and even allergy meds. Many contain ingredients that interact with St. John’s Wort.
- Talk to your pharmacist. They’re trained to spot interactions. Bring your pill bottles or a list of everything you take. Ask: “Could any of these interact with St. John’s Wort?”
- Ask about alternatives. SAM-e and 5-HTP have far fewer interactions. While they’re not as well studied for depression, they’re much safer if you’re on other meds.
- Consider therapy. Cognitive behavioral therapy (CBT) is as effective as St. John’s Wort for mild depression, with zero interaction risks.
If you’re already taking St. John’s Wort and you’re on any prescription drug, don’t stop suddenly. Talk to your doctor. Stopping abruptly can cause withdrawal symptoms like dizziness or irritability. But don’t wait until something goes wrong. Get checked now.
The Bottom Line
St. John’s Wort isn’t a harmless herb. It’s a potent drug that changes how your body processes other drugs. For people who aren’t on any medications, it might help with mild depression. But if you take pills-any pills-it’s a gamble with your life. The consequences aren’t just side effects. They’re organ rejection, unintended pregnancy, seizures, and death.
There’s no safe middle ground. Either you’re on no medications, or you shouldn’t take it. No exceptions. No “I’ll just take a little.” No “I didn’t know.” The science is clear. The warnings are out there. The risk isn’t worth it.
Can I take St. John’s Wort if I’m on birth control?
No. St. John’s Wort reduces estrogen levels in your body, which can make hormonal birth control ineffective. There are documented cases of women becoming pregnant while on the pill and taking St. John’s Wort. Even if your period seems normal, your protection could be gone. Use a backup method like condoms, or switch to a non-hormonal option like a copper IUD.
How long does it take for St. John’s Wort to start interacting with my meds?
It can take as little as 5-7 days for enzyme induction to begin, with full effects peaking around 10-14 days. That’s why people often don’t realize something’s wrong until weeks later-when their transplant drug levels drop or their antidepressant stops working. The effects also last for up to two weeks after you stop taking St. John’s Wort, so timing matters even if you plan to quit.
Is there a safe version of St. John’s Wort without interactions?
Researchers are testing low-hyperforin extracts that reduce enzyme induction by up to 90%. These aren’t available to the public yet. Even if they were, they’d still need to be tested with every medication you take. Until then, assume all St. John’s Wort products carry the same risks.
Can I take St. John’s Wort if I’m not on any prescriptions?
It’s still risky. Many people take over-the-counter meds like ibuprofen, antacids, or cold medicines without realizing they can interact. St. John’s Wort can affect liver enzymes that process these too. Plus, it can cause its own side effects-dry mouth, dizziness, anxiety, and increased sun sensitivity. If you’re not on meds, it’s safer to try therapy, exercise, or light therapy for depression instead.
What should I do if I’ve already taken St. John’s Wort with my meds?
Stop taking it immediately and contact your doctor or pharmacist. Don’t wait for symptoms. Ask for blood tests to check levels of your medications-especially if you’re on transplant drugs, warfarin, or HIV meds. Keep taking your prescriptions unless told otherwise. Your provider may need to adjust your dose or monitor you closely for the next few weeks.
Paige Lund
So… let me get this straight. Natural = dangerous, and pills = safe? Cool, cool. I’ll just keep my Prozac and skip the herb. 🤷♀️
Reema Al-Zaheri
St. John’s Wort’s mechanism of action-via PXR-mediated upregulation of CYP3A4, CYP2C9, and CYP1A2-is well-documented in peer-reviewed pharmacokinetic studies. The clinical implications are not speculative; they are empirically validated across multiple case series. This is not anecdotal-it is evidence-based pharmacology.
Richard Risemberg
Man, I used to swear by this stuff-until my buddy’s cousin’s neighbor got her kidney rejected because she thought ‘herbal’ meant ‘harmless.’ I’m not saying don’t try natural remedies-I’m saying don’t be a dumbass with your liver. Talk to your pharmacist. Bring your whole damn medicine cabinet. They’ve seen worse. And they won’t judge you-until you tell them you mixed it with warfarin and didn’t think twice.
Andrew Montandon
Let’s be real: if you’re taking anything that keeps you alive-transplant meds, blood thinners, HIV drugs-you’re not ‘just trying a supplement.’ You’re playing Russian roulette with your biology. And no, ‘I only took it for a week’ doesn’t matter-this stuff lingers. It’s like a ghost in your liver that won’t leave. Stop pretending it’s just tea. It’s a drug. A sneaky, sneaky drug.
Sam Reicks
the fda is just in bed with big pharma and they hate natural stuff because it dont make em money. st johns wort is fine. its the pills that are the real problem. why do you think they dont let you sell it in europe? because they want you hooked on expensive drugs. its all a scam. i took it for 5 years and my blood pressure is better than ever. they just dont want you to know the truth.
Frank Dahlmeyer
Let me tell you, I’ve spent the last three years researching herbal interactions because my sister almost lost her lung transplant after taking St. John’s Wort for ‘a little anxiety.’ I read every journal, every case study, every FDA advisory. And let me tell you-this isn’t just about drug interactions. It’s about systemic negligence. We treat herbs like candy and pharmaceuticals like divine interventions, when in reality, both are chemicals with consequences. We need regulation. We need labeling. We need education. And until then, people are going to keep dying because someone thought ‘natural’ meant ‘no side effects.’
Angela Gutschwager
So… don’t take it if you’re on meds. Got it. 🙄
Dion Hetemi
Here’s the real issue: people think they’re ‘taking control’ of their health by self-medicating with herbs, but they’re just handing over their biology to a $20 bottle of questionable extract with no oversight. And then they act shocked when their birth control fails. Surprise! Your body isn’t a TikTok algorithm. It doesn’t ‘choose’ what works. It follows biochemistry. And biochemistry doesn’t care how ‘clean’ your lifestyle is.
Kara Binning
THIS IS WHY AMERICA IS FALLING APART. We let unregulated, untested, ‘hippie magic’ potions sit next to aspirin like it’s 1999. Meanwhile, in Germany, they have warnings on the bottle. In the U.S., you need a PhD to read the tiny disclaimer on the back. This isn’t freedom. This is negligence. And someone’s gonna die because their pharmacy didn’t care enough to warn them. And then the lawsuit will happen. And then they’ll say ‘we didn’t know.’ Well, now you know. And you’re still buying it. You’re part of the problem.
river weiss
As a clinical pharmacist with over 18 years in practice, I’ve seen too many patients come in with undiagnosed serotonin syndrome, transplant rejection, or unexplained clotting events-all because they assumed St. John’s Wort was ‘safe.’ I always ask: ‘Are you taking anything herbal?’ And 90% of the time, they say ‘no.’ They don’t even consider it medicine. It’s not. It’s a pharmacologically active compound with a half-life, a metabolic pathway, and documented interactions with over 50 medications. If you’re on anything-anything-check with your pharmacist before touching it. Don’t wait for a crisis.
Brian Rono
St. John’s Wort is the gateway herb to pharmaceutical anarchy. You start with it because you ‘hate pills,’ then you add ashwagandha, then CBD, then melatonin, then turmeric, then ‘that tea your yoga teacher swears by.’ Suddenly your liver is a war zone and your doctor’s like, ‘Why is your INR at 0.8?’ Because you thought ‘natural’ meant ‘no consequences.’ Spoiler: it doesn’t. Nature doesn’t care if you’re ‘healing.’ It just metabolizes. And it doesn’t ask permission.
seamus moginie
Look, I’m Irish-we’ve been using herbs for centuries. But I’ll tell you this: if your grandad took St. John’s Wort and lived to 92, that doesn’t mean it’s safe for you. Times change. Medicines change. Your body’s not his. And if you’re on anything prescribed? Don’t be a hero. Talk to someone who knows. I’ve seen too many people die because they thought ‘tradition’ meant ‘science.’ It doesn’t.
Dana Dolan
My mom took this for depression and didn’t tell her doctor she was on levothyroxine. She ended up in the ER with myxedema. She’s fine now, but she’s terrified of supplements. I just wish someone had told her before she started.
Codie Wagers
It’s not about St. John’s Wort. It’s about the illusion of autonomy in a medical system that commodifies health. We’re told to ‘take charge’-but the moment we do, we’re blamed when things go wrong. The real failure isn’t the herb-it’s the lack of regulation, the absence of mandatory labeling, the corporate indifference to consumer safety. The FDA doesn’t regulate supplements because it’s profitable to let them slide. And we, the consumers, are the collateral damage in a system that treats biology like a marketplace. This isn’t about ignorance. It’s about design.
Michael Petesch
As a medical professional practicing in the U.S., I would like to emphasize that the pharmacological profile of St. John’s Wort is not merely a theoretical concern-it is a documented, clinically significant, and preventable public health issue. The herb’s induction of hepatic cytochrome P450 enzymes and P-glycoprotein transporters results in clinically relevant reductions in plasma concentrations of numerous medications, including but not limited to cyclosporine, tacrolimus, warfarin, and oral contraceptives. The consequences are not hypothetical; they are fatal. The absence of mandatory warning labels in the United States represents a critical gap in patient safety infrastructure. I strongly urge all patients to disclose all herbal supplement use to their prescribing clinicians and pharmacists. The burden of safety should not rest solely on the individual. Systemic reform is necessary.