After losing a limb, many people still feel pain in the part that’s no longer there. This isn’t imagination. It’s real. It’s called phantom limb pain, and it affects 60% to 85% of amputees. The pain can feel like burning, stabbing, cramping, or tingling deep in the missing foot, hand, or leg. For some, it fades after a few months. For others, it sticks around - sometimes for years. And if it lasts longer than six months, the chance of it disappearing on its own is nearly zero.
Why Does Phantom Limb Pain Happen?
It’s not in the stump. It’s in the brain. When a limb is amputated, the nerves that once sent signals from that limb to the brain don’t just disappear. They keep firing. The brain, still expecting input from the missing limb, misinterprets those signals as pain. Imaging studies show that areas of the brain once responsible for sensing the amputated limb light up during episodes of phantom pain. This isn’t psychological. It’s neurological rewiring. The brain tries to adapt. Neighboring areas - like the face or torso - start taking over the space once used by the missing limb. That’s why touching your cheek might trigger a sharp pain in your phantom hand. This process, called cortical remapping, is one of the main reasons the pain becomes stubborn. Risk factors make it worse. If you had chronic pain in the limb before amputation, or if you had severe pain right after surgery, you’re far more likely to develop long-term phantom pain. Tumor-related amputations also carry higher risk. Even things like stress, cold weather, or an ill-fitting prosthetic can trigger flare-ups.Medications: What Works and What Doesn’t
Most people start with medication. It’s the most common first step. But not all drugs work the same for everyone. What helps one person might do nothing for another. Tricyclic antidepressants like amitriptyline and nortriptyline are the most commonly prescribed. They’re not used because the patient is depressed. They work by calming overactive nerve signals. A typical starting dose is 10 mg at bedtime, slowly increased over weeks. About 45% of users report moderate relief, but side effects like drowsiness, dry mouth, and weight gain cause many to quit. Anticonvulsants like gabapentin and pregabalin are next in line. Originally for seizures, they’re great at blocking nerve pain. Gabapentin often starts at 300 mg a day and can go up to 3,600 mg. Pregabalin works faster and is dosed between 75 and 600 mg daily. On Reddit’s amputee forum, 72% of users said gabapentin helped - but 58% stopped because of dizziness or brain fog. NSAIDs like ibuprofen and naproxen give mild, short-term relief. About 65% of users feel better at first, but after three to six months, 80% say the effect fades. They’re not a long-term solution. For tough cases, doctors may turn to NMDA antagonists like ketamine, given intravenously in small doses. It’s powerful but comes with risks: hallucinations, high blood pressure, and potential for abuse. It’s not for everyone. Opioids like oxycodone and morphine are used only when nothing else works. They’re controversial. The American Pain Society recommends keeping daily doses under 50 morphine milligram equivalents (MME) because of addiction risk. On pain forums, 35% of long-term opioid users report dependence issues. A newer option is botulinum toxin (Botox) injections into the residual limb. For patients with painful neuromas (tangled nerves), one injection can reduce pain from 8/10 to 3/10 for up to 12 weeks. It’s not widely available, but it’s showing real promise.Mirror Therapy: Seeing Is Believing
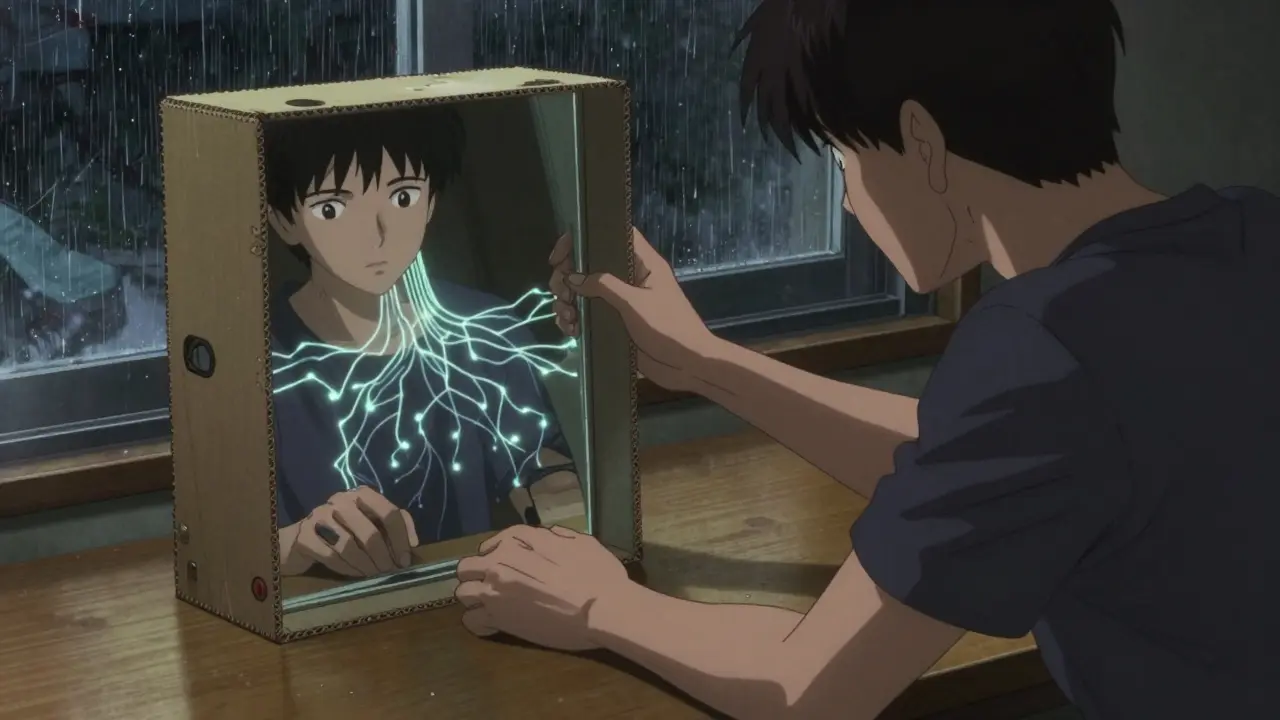
Mirror therapy is one of the most surprising, non-drug treatments for phantom pain. It was pioneered by neuroscientist V.S. Ramachandran, who noticed that visual feedback could trick the brain into thinking the missing limb was moving again - and that this could stop the pain signals. Here’s how it works: You sit with a mirror standing vertically between your intact limb and your stump. You move your good hand while watching its reflection in the mirror. To your brain, it looks like the missing limb is moving too. Over time, this visual feedback helps rewire the brain’s misfiring pathways. You need to do it daily - 15 to 30 minutes, five to seven days a week. Some people use a mirror box, others make one with a cardboard box and a piece of glass. It sounds simple. But sticking with it is hard. Studies show 40% of people quit within eight weeks because they don’t see results fast enough. Success isn’t guaranteed. But for those who stick with it, relief can be real. One 2023 study found that 60% of patients who practiced mirror therapy daily for eight weeks reported at least a 50% drop in pain intensity. And unlike pills, there are no side effects.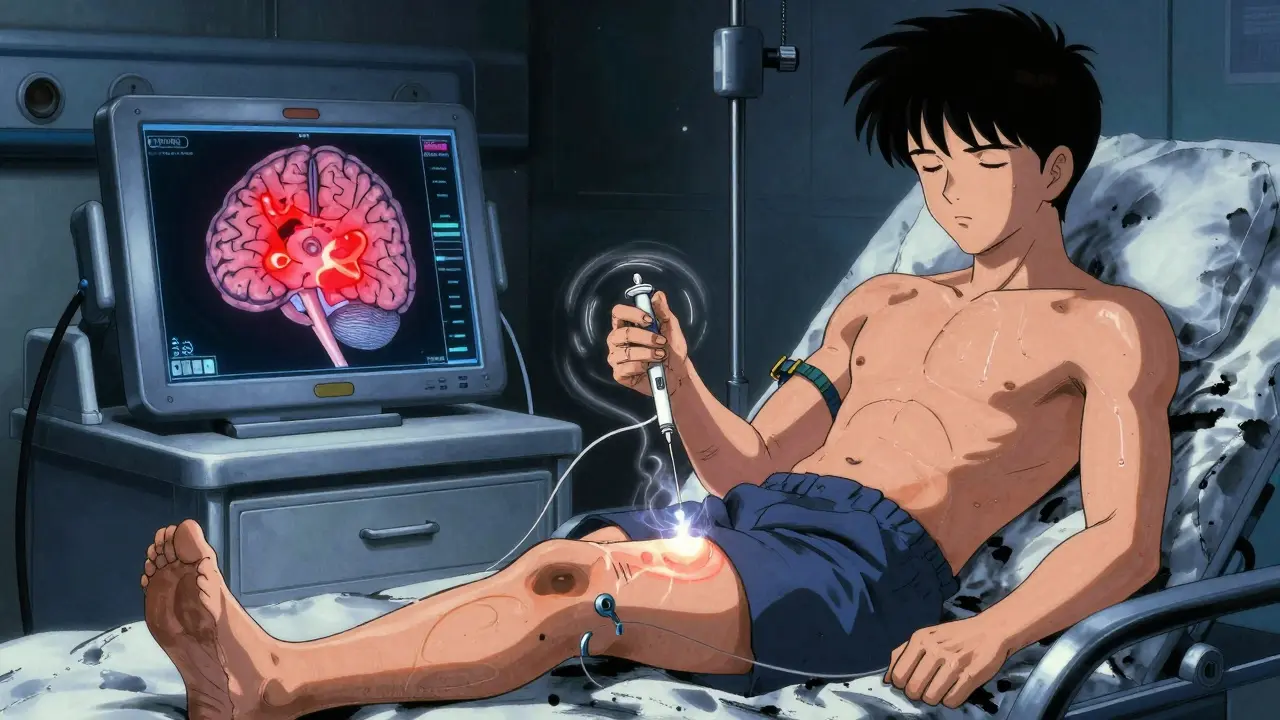
Other Non-Medication Options
If medications and mirrors aren’t enough, other tools exist:- TENS (Transcutaneous Electrical Nerve Stimulation): Electrodes taped to the stump deliver tiny electrical pulses. It works for 30-50% of users. You need proper training - wrong settings can make it worse.
- Spinal Cord Stimulation: A small device implanted near the spine sends pulses to block pain signals. It’s for severe, long-term cases. Success rates are 40-60%.
- Biofeedback: Teaches you to control body functions like muscle tension and heart rate. Helps 25-40% of people manage pain better.
- Virtual Reality (VR): The next step beyond mirrors. Instead of a physical mirror, you wear VR goggles and see a digital version of your missing limb moving in sync with your good limb. Early trials show it boosts adherence - and pain relief - by making therapy feel more engaging. By 2027, experts predict VR will increase mirror therapy success rates from 60% to 85%.
What Doesn’t Work (And Why)
Some treatments get a lot of attention but don’t deliver. Epidural anesthesia during amputation was once thought to prevent phantom pain. But research now shows it doesn’t. Neither do acupuncture or herbal supplements - no solid evidence supports them. Also, don’t expect one magic drug. Most people need a mix. A 2024 review in the Journal of Neurosurgery found that combining mirror therapy with a low-dose anticonvulsant worked better than either alone. That’s the future: layered, personalized care.When to Seek Help
Don’t wait. If you’ve had phantom pain for more than six months, it won’t go away without action. Early intervention is key. Start with your doctor or a pain specialist. Ask about:- Trial of amitriptyline or gabapentin
- Getting a mirror box and learning how to use it
- Referral to a physical therapist trained in phantom pain
- Checking if you’re a candidate for TENS or spinal stimulation

What to Expect Long-Term
Phantom limb pain isn’t curable. But it’s manageable. The goal isn’t to erase every twinge - it’s to reduce pain enough to live well. With the right mix of meds, mirror therapy, and support, most people can cut their pain by half or more. New tech is coming. The FDA approved a smart spinal stimulator called Evoke in January 2024. It adjusts automatically based on your pain levels. Clinical trials showed 65% average pain reduction. And drug companies are testing new NMDA blockers that work like ketamine but without the side effects. The big shift? Moving away from pills alone. The future is combination therapy: medication for quick relief, mirror therapy or VR for long-term brain rewiring, and support groups to keep you going.Real Stories, Real Results
One man in Perth started mirror therapy six months after his leg amputation. At first, he thought it was silly. After three weeks, he noticed the burning sensation in his toes eased. By month two, he was sleeping through the night. He still takes gabapentin, but his dose is half what it was. Another woman in Brisbane tried six different drugs before her doctor suggested Botox. One injection reduced her pain from 9/10 to 4/10. She says it gave her back her life - she started walking again, went back to gardening. They didn’t find one solution. They found the right mix.Where to Find Support
You’re not alone. The Amputee Coalition supports over 12,000 people a year with peer networks, educational materials, and therapy guides. Online forums like r/amputee on Reddit offer real talk from people who’ve been there. You don’t have to suffer in silence. Help exists. And it’s getting better every year.Is phantom limb pain all in my head?
No. Phantom limb pain is real and has a clear neurological basis. Brain scans show activity in areas that once controlled the missing limb. It’s not psychological - it’s a result of nerve and brain changes after amputation.
How long does phantom limb pain last?
For many, it fades within six months. But if it lasts longer than that, the chance of it going away on its own is nearly zero. Persistent pain needs active treatment. Waiting won’t help.
Can mirror therapy really help?
Yes. Studies show about 60% of people who practice mirror therapy daily for 4-8 weeks see at least a 50% reduction in pain. It works by tricking the brain into thinking the missing limb is moving again, helping rewire faulty pain signals.
What’s the best medication for phantom limb pain?
There’s no single best drug. Tricyclic antidepressants like amitriptyline and anticonvulsants like gabapentin are first-line treatments. Effectiveness varies by person. Many need to try 2-3 options before finding one that works. Always start low and increase slowly under medical supervision.
Are opioids safe for phantom limb pain?
Opioids like oxycodone are sometimes used for severe cases, but they carry high risks of dependence and side effects. Experts recommend limiting daily doses to under 50 morphine milligram equivalents (MME) and only using them when other treatments fail. They’re not a long-term solution.
Can I do mirror therapy at home?
Yes. You can buy a mirror box or make one with a cardboard box and a mirror. Sessions should last 15-30 minutes, once or twice daily. It’s simple, but consistency matters. Most people who quit do so because they don’t see results fast enough - stick with it for at least four weeks.
What’s new in phantom pain treatment?
In early 2024, the FDA approved a new spinal cord stimulator called Evoke that adjusts automatically to your pain levels, showing 65% average pain reduction. Virtual reality versions of mirror therapy are also being tested and may boost adherence. Research into safer NMDA blockers could replace ketamine in the near future.
How do I know if I need a pain specialist?
If you’ve tried one or two medications without relief, or if your pain is interfering with sleep, movement, or daily life, it’s time to see a pain specialist. Many major hospitals now have dedicated phantom limb pain clinics with teams that combine meds, therapy, and tech for better outcomes.
Jacob Cathro
so like... i tried mirror therapy for 2 weeks and it felt like watching my hand do yoga while my leg screamed in hell. i didn’t get no relief, just a weird mirror addiction. why is this even a thing? someone’s selling these boxes on amazon for $80. lmao.
Paul Barnes
There is a grammatical error in the third paragraph: ‘It’s not in the stump. It’s in the brain.’ is correctly punctuated, but the following sentence begins with ‘When a limb is amputated, the nerves that once sent signals from that limb to the brain don’t just disappear.’ - this is technically correct, but the subject-verb agreement is unnecessarily convoluted. Precision matters in medical communication.
pragya mishra
Why are you not talking about the real solution? Acupuncture works. I did it in Delhi. I had phantom pain for 3 years. One session and it was 70% gone. Why are doctors ignoring this? Because Big Pharma doesn’t own it. You’re being lied to. Try it. I dare you.
Andy Thompson
mirror therapy? lol. that’s just the government’s way of making us think we’re healing while they monitor our brainwaves through the mirror. next thing you know, they’ll be syncing it with NSA satellites. i’ve seen the footage. they’re watching us try to move our phantom legs. and don’t even get me started on Botox… it’s a mind-control agent disguised as a cosmetic treatment. 😈
sagar sanadi
gabapentin? yeah right. i took it for a month. felt like my brain was made of wet socks. then i found out the real cause: aliens stole my leg and left a psychic echo. they’re still testing it. the pain only stops when the moon is full. ask me how i know.
kumar kc
If you’re still in pain after six months, you’re not trying hard enough. Just pray and stop complaining.
Shane McGriff
I’ve been living with this for 8 years. Started with gabapentin, then mirror therapy, then TENS. Nothing worked alone. But combining mirror therapy with low-dose nortriptyline? Game-changer. I can sleep again. I can walk without bracing for pain. It’s not perfect - but it’s progress. Don’t give up. Try one thing at a time. And if you’re stuck, DM me. I’ve been there.
Art Gar
It is imperative to note that the empirical validity of mirror therapy remains contingent upon methodological rigor in clinical trials. While anecdotal reports abound, the absence of double-blind, placebo-controlled studies with sufficient statistical power renders the purported efficacy of this intervention speculative at best. One must exercise caution before endorsing non-pharmacological modalities lacking robust peer-reviewed substantiation.
Crystal August
Why do we always assume the brain is the problem? What if the pain is actually the limb’s ghost screaming for justice? We cut it off. It’s still alive in some way. We should be apologizing, not prescribing.
Nadia Watson
I’m from the U.S., but my cousin in Kerala tried mirror therapy with a polished steel plate and a cardboard box - no fancy gear. He did it every morning while sipping chai. After 6 weeks, his burning stopped. He still takes gabapentin, but now he’s gardening again. Sometimes the simplest things work best. Just don’t give up. 💪
thomas wall
It is deeply concerning that society continues to treat phantom limb pain as a mere neurological anomaly, rather than a profound existential rupture. The limb is not merely absent - its memory haunts the somatosensory cortex. To reduce this to pharmacological management or optical illusions is to deny the dignity of the amputee’s lived experience. We must elevate the discourse beyond the laboratory.
Manoj Kumar Billigunta
Hey, I’ve been there. Mirror therapy felt stupid at first too. But I stuck with it - 15 minutes a day, no excuses. After 3 weeks, the stabbing in my toes started fading. Now I do it while watching Netflix. No magic. Just consistency. And if you’re on meds, don’t quit cold turkey. Talk to your doc. You’re not alone. I’m here if you wanna chat.