Peanut allergy used to be seen as a life-long sentence. A child diagnosed with it faced strict avoidance, emergency epinephrine on hand at all times, and the constant fear of accidental exposure. But that’s no longer the whole story. In the last decade, science has flipped the script. We now know that peanut allergy isn’t inevitable - and in many cases, it can be prevented before it even starts.
What Changed? The LEAP Study That Rewrote the Rules
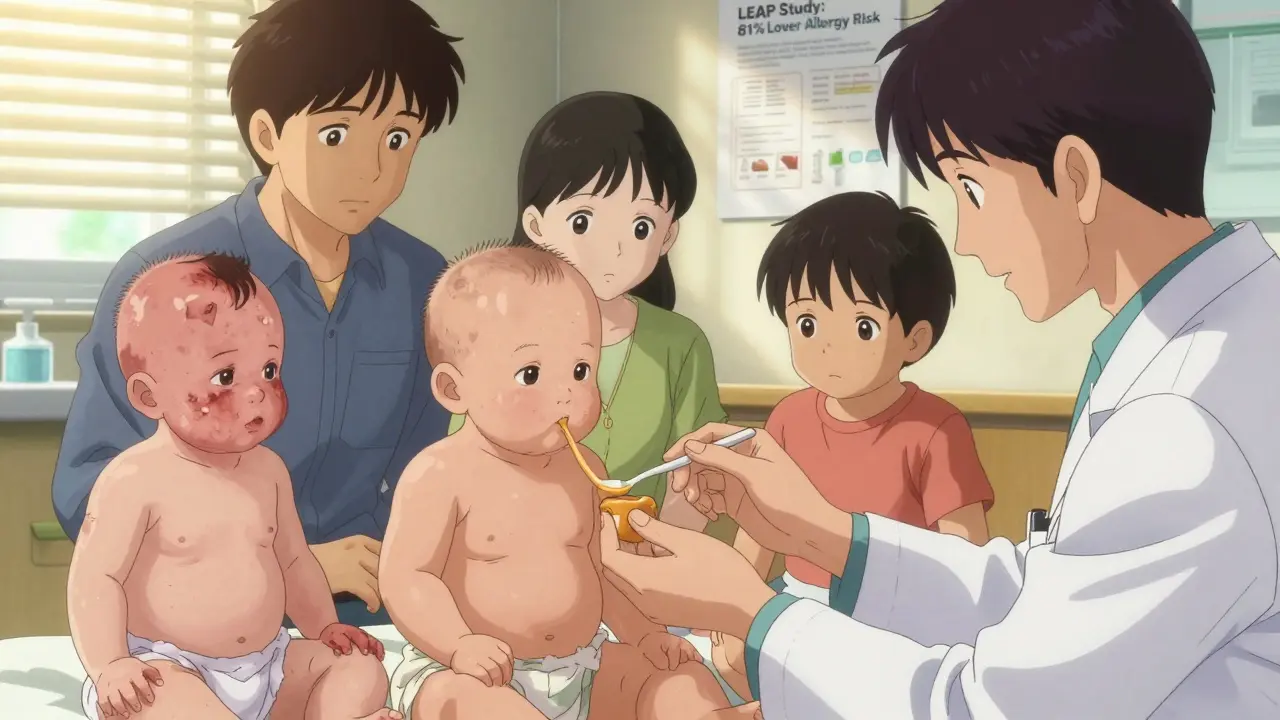
Before 2015, doctors told parents to wait. If your baby had eczema or an egg allergy - signs they might be more prone to allergies - you were advised to hold off on peanuts until age two or three. The thinking was simple: delay exposure, reduce risk. But the numbers told a different story. Between 1997 and 2010, peanut allergies in U.S. children more than quadrupled, from 0.4% to 2.0%. Something wasn’t adding up. Then came the LEAP study - Learning Early About Peanut Allergy. Led by Dr. Gideon Lack at King’s College London, this landmark trial followed over 600 high-risk infants from infancy to age five. Half were told to avoid peanuts entirely. The other half were given small, regular doses of peanut protein starting between 4 and 11 months of age. By age five, the results were staggering: the group that ate peanut early had an 81% lower rate of peanut allergy. The difference wasn’t small. It was revolutionary. The findings didn’t sit on a shelf. In 2017, the National Institute of Allergy and Infectious Diseases (NIAID) released new guidelines, backed by 26 major medical groups. They didn’t just suggest early introduction - they made it a standard of care.How to Introduce Peanut Based on Risk Level
The current guidelines aren’t one-size-fits-all. They’re built on three clear risk categories:- High-risk infants: Those with severe eczema, egg allergy, or both. These babies should be evaluated by a doctor or allergist between 4 and 6 months. If testing shows no peanut sensitivity, peanut protein is introduced under medical supervision, then continued at home three times a week.
- Moderate-risk infants: Those with mild to moderate eczema. No testing is needed. Start peanut-containing foods around 6 months, at home, in a safe form.
- Low-risk infants: No eczema or food allergies. Introduce peanut anytime after starting solids, usually around 6 months, just like any other food.
Oral Immunotherapy (OIT): Treating, Not Preventing
It’s important to understand: early introduction is about prevention. Oral Immunotherapy (OIT) is about treatment. OIT is for children who already have a diagnosed peanut allergy. It involves giving tiny, increasing amounts of peanut protein under strict medical supervision, slowly building tolerance. The goal isn’t to cure the allergy - it’s to reduce the chance of a life-threatening reaction from accidental exposure. Studies show that after months of daily dosing, many kids can safely eat a few peanuts without a reaction. But it’s not risk-free. Side effects like stomach upset, hives, or even anaphylaxis can happen. That’s why OIT is only done in specialized clinics, not at home. The American College of Allergy, Asthma, and Immunology (ACAAI) is clear: OIT is not a substitute for early introduction. It’s a different tool for a different problem. You don’t need OIT if you prevent the allergy in the first place.
Why So Many Parents Still Don’t Do It
Despite the science, adoption is lagging. A 2022 study found that only about 39% of high-risk infants in the U.S. actually received early peanut introduction. Why? Parents are scared. They’ve been told for years that peanuts are dangerous. Now they’re being asked to give them to a baby who might be at risk. The anxiety is real. One survey showed 62% of parents worried about a reaction during the first introduction. Doctors aren’t always on the same page either. A 2023 survey found that only 54% of pediatricians could correctly describe the current guidelines. Some still tell parents to wait. Others don’t know how to help families get started safely. And then there’s access. Not every family can easily get to an allergist. Not every pediatrician has the time or training to guide them through it. And cultural or language barriers make it even harder. The result? A gap in outcomes. A 2023 study showed that Black and Hispanic infants were 22% less likely to receive early peanut introduction than White infants - contributing to ongoing disparities in allergy rates.What Works - and What Doesn’t
You’ll hear a lot of theories about preventing food allergies. Eat more yogurt during pregnancy? Take vitamin D? Use probiotics? None of them hold up. Cochrane reviews - the gold standard for evaluating medical evidence - found no clear benefit from maternal diet changes, probiotics, or vitamin D supplements for preventing peanut allergy. The only intervention with strong, consistent, repeatable results? Early introduction of peanut protein. Even more telling: the protection lasts. Follow-up from the original LEAP study showed that even after a full year of avoiding peanuts, kids who had eaten them early still remained protected. That’s not just desensitization - it’s true immune tolerance. The body learned to accept peanut as safe.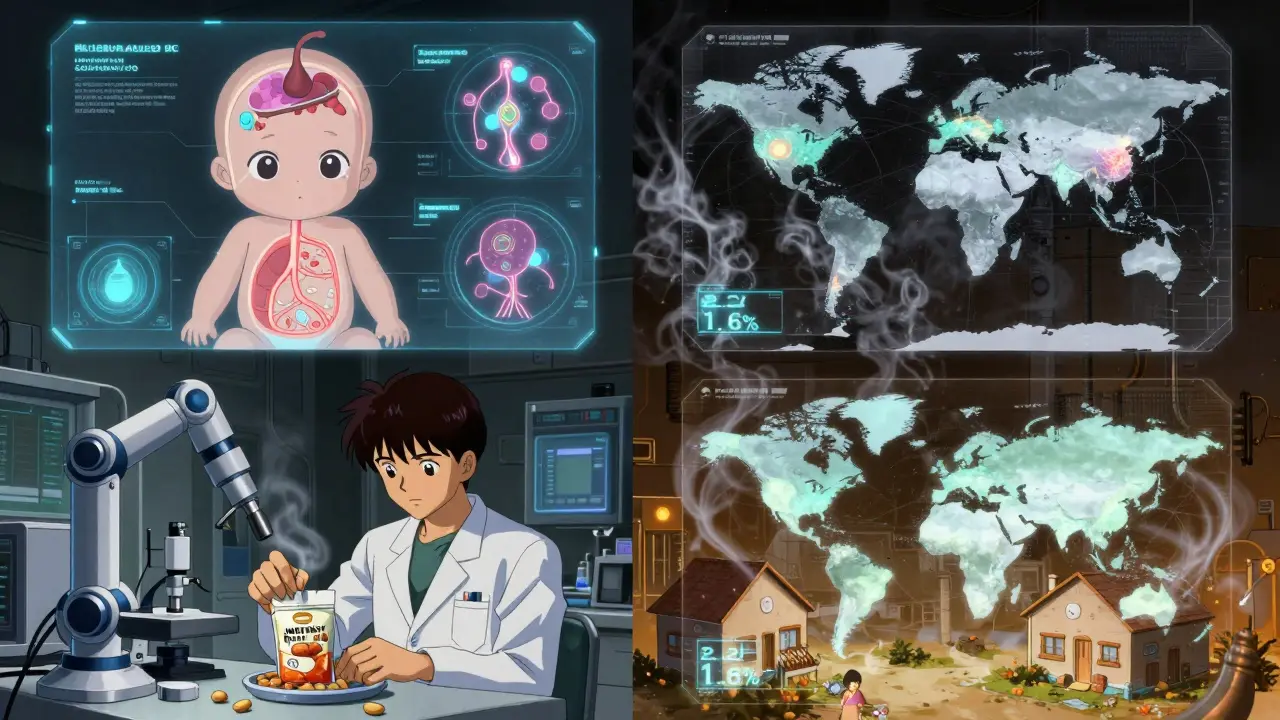
What’s Next? The Future of Prevention
Researchers are now looking beyond peanut. The EAT study extension showed that introducing multiple allergens - peanut, egg, milk, and others - early on may protect against more than one allergy at once. The Consortium of Food Allergy Researchers (COFAR), funded by the NIAID, is running the PRESTO trial right now, testing the best timing and dose for high-risk babies. Results are expected in 2026. Meanwhile, the market is catching up. Peanut butter pouches, infant peanut snacks, and ready-to-use peanut powders are now widely available. Sales of these products have grown 27% annually since 2018. Companies are responding to demand - and families are finally getting the tools they need. The CDC reports that peanut allergy rates have already dropped from 2.2% in 2015 to 1.6% in 2023. That’s roughly 300,000 fewer children with peanut allergies. If early introduction rates climb from 39% to 65% among high-risk infants - as experts predict - GlobalData forecasts peanut allergy rates could fall to 1.2% by 2030.What Parents Should Do Right Now
If you’re expecting a baby or have a child under 12 months:- Look at your baby’s skin. Do they have severe eczema? Have they been diagnosed with egg allergy? If yes, talk to your pediatrician by 3-4 months. Ask about referral to an allergist.
- If your baby has mild or moderate eczema, start peanut around 6 months. No testing needed. Just make sure it’s smooth peanut butter, mixed thin, or an approved infant product.
- If your baby has no eczema or food allergies, introduce peanut when you start solids - no rush, no fear.
- Never give whole peanuts, chunks, or sticky peanut butter straight from the jar. Always mix it into a thin puree.
- Start with a small amount. Watch for signs of reaction: hives, vomiting, swelling, trouble breathing. If anything happens, stop and call your doctor.
- Keep going. Three times a week, every week. Consistency matters more than the amount.
Can I introduce peanut butter to my 4-month-old?
Yes - but only if your baby is at high risk for peanut allergy (severe eczema or egg allergy) and has been cleared by a doctor. For high-risk babies, the first peanut exposure should happen between 4 and 6 months, ideally under medical supervision. For other babies, wait until they’re ready for solids, usually around 6 months. Always use smooth peanut butter mixed with water or breast milk - never whole peanuts or thick globs.
Is oral immunotherapy (OIT) the same as early introduction?
No. Early introduction is for babies who don’t have a peanut allergy yet - it’s a prevention strategy. OIT is for children who already have a diagnosed peanut allergy. OIT slowly builds tolerance to reduce the risk of severe reactions from accidental exposure, but it’s not a cure and requires ongoing medical supervision. You don’t need OIT if you prevent the allergy early.
What if my baby has a reaction to peanut?
Stop giving peanut immediately. If the reaction is mild - like a few hives or a rash - call your pediatrician. If it’s severe - swelling of the lips or tongue, vomiting, trouble breathing, or loss of consciousness - use epinephrine if you have it and call 911. Never ignore a reaction. Even if it seems small, follow up with an allergist to confirm whether it was truly an allergy.
Can I use natural peanut butter with added oil or sugar?
Yes - as long as it’s smooth and contains only peanuts (and maybe salt). Avoid peanut butter with added honey (not safe under age 1), chocolate, or excessive sugar. The goal is to give peanut protein, not a sugary snack. Stick to simple, unflavored, smooth peanut butter. If you’re unsure, check the label: ingredients should say “peanuts” or “peanuts and salt.”
Do I need to keep feeding peanut forever once I start?
Yes. Consistency is key. The guidelines recommend feeding peanut protein at least three times a week, long-term. Stopping after a few weeks or months may reduce the protective effect. You don’t need to give it every day - just regularly. Many families find it easiest to mix peanut butter into oatmeal, yogurt, or pureed fruits on a few days each week.
Kacey Yates
Just gave my 5-month-old peanut butter mixed in oatmeal after the doc said it was fine. No reaction. Feels like we dodged a bullet. Seriously, why are we still scared of food? 😅
Ryan Pagan
Man, this is the kind of science that actually matters. We’ve been running on fear-based parenting for decades - ‘don’t give them anything until they’re 2’ - and it backfired spectacularly. Early exposure isn’t just smart, it’s a public health win. The fact that we’re seeing real drops in allergy rates now? That’s not coincidence. That’s evidence working. Time to stop treating peanut butter like it’s a landmine.
Doug Gray
Interesting how the same people who demand ‘natural’ parenting suddenly panic when you suggest introducing a common food before 12 months. It’s not magic, it’s immunology. But sure, let’s keep blaming GMOs and vaccines while 300k fewer kids have allergies. 🤷♂️
ryan Sifontes
They’re testing this on babies but won’t tell you what’s in those peanut pouches. Who’s funding this? Big Peanut? The FDA? The same folks who said smoking was safe? I’m not letting my kid near anything labeled ‘for infants’ that wasn’t around in 1990.
Laura Arnal
This made me cry. My son had a severe reaction at 11 months and we were terrified for years. Now I’m telling every new parent I know: DON’T WAIT. It’s not risky - it’s the opposite. You’re giving them freedom. 🤍
Jasneet Minhas
As someone from India where peanut chutney is in every kitchen since birth - this is hilarious. We’ve been doing this for centuries. Now Western medicine ‘discovers’ it? 🤭
Eli In
My mom is from Nigeria - she fed my brother peanut paste at 6 months like it was rice cereal. He’s 28 now and has never had an allergy. Meanwhile, my cousin in Ohio was told to wait until 3. He’s allergic. Culture matters. Science just caught up.
Sheryl Dhlamini
But what if the immune system isn’t being ‘trained’ - what if it’s being hijacked by industrialized food systems, glyphosate-laced peanut butter, and the corporate agenda to sell more ‘infant-safe’ peanut products? Are we really sure this isn’t just another form of controlled exposure designed to normalize dependency on processed foods under the guise of ‘prevention’? The LEAP study was funded by… well, you know who. And the follow-up? No independent replication. Just corporate-backed echo chambers. We’re being sold a narrative disguised as medicine.
Megan Brooks
While the data is compelling, the implementation gap is staggering. Families without access to allergists, or those navigating language barriers, are being left behind. This isn’t just a medical issue - it’s a social equity crisis. Guidelines mean nothing if they’re only accessible to those who can afford to ask the right questions.
Paul Adler
My pediatrician didn’t even mention this until I brought it up. I had to Google it myself. That’s the real problem here - not the science, but the disconnect between research and frontline care. We need better training, not just better guidelines.
Robin Keith
Let’s be real - if this were about preventing allergies to something less profitable than peanut butter - say, broccoli - would we be having this conversation? Would the AAP be issuing guidelines? Would there be pouches on every shelf? No. This is capitalism disguised as prevention. The fact that peanut allergy rates are dropping is great - but let’s not pretend the profit motive isn’t driving the messaging. We’re being sold a solution that only works if you buy the product. And don’t get me started on the ‘three times a week’ requirement - that’s not medicine, that’s a subscription model.