Medication Side Effect Calculator
Select your condition to see which delivery method has the lowest side effect risk based on medical evidence.
Your Best Option
Oral
75% of all medications
Injection
1-5% site reactions
Topical
15-20% local reactions
When you take a pill, get a shot, or rub on a cream, you’re not just choosing how to take your medicine-you’re choosing how your body reacts to it. The route of administration isn’t just a technical detail. It shapes everything: how fast the drug works, how much of it actually gets into your system, and most importantly, what kind of side effects you’re likely to face. Many people assume all medications work the same no matter how they’re given. That’s not true. In fact, the difference between taking a drug by mouth, injecting it, or applying it to your skin can mean the difference between mild nausea and a serious reaction.
Oral Medications: Convenient, But Hard on the Gut
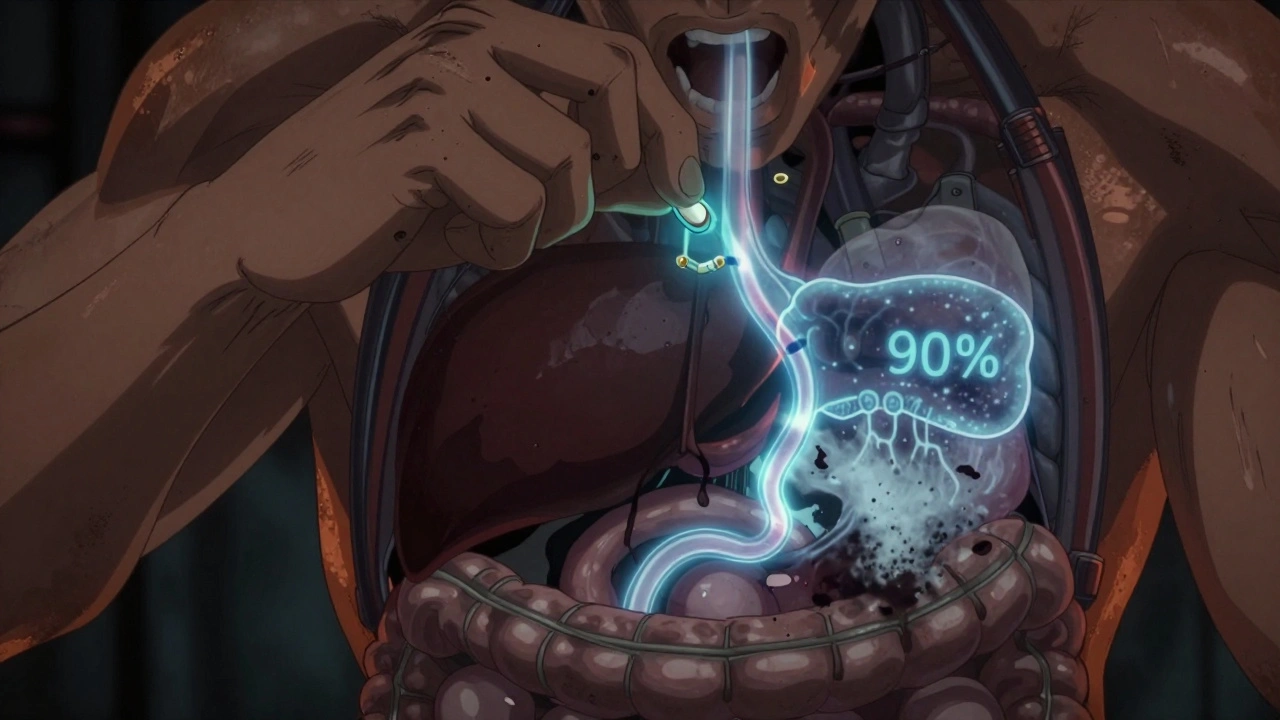
Over 75% of all medications are taken by mouth. It’s easy. No needles. No mess. Just swallow a pill with water. But that convenience comes at a cost. When you take a drug orally, it has to survive your stomach acid, get absorbed through your intestines, and then pass through your liver before it ever reaches your bloodstream. This is called first-pass metabolism, and it can destroy up to 90% of some drugs before they even start working.
Take propranolol, a common heart medication. Only about 25% of the dose you swallow actually makes it into your system. To make up for that loss, doctors prescribe higher doses-which means more of the drug is floating around your body, increasing the chance of side effects. That’s why stomach upset, nausea, and diarrhea are so common with oral meds. NSAIDs like ibuprofen cause stomach ulcers in 1-2% of long-term users. That’s not rare. That’s expected.
And it’s not just the stomach. Food changes everything. Forty percent of common prescriptions interact with meals. Grapefruit juice can turn a safe dose of a cholesterol drug into a dangerous one. Antacids can block absorption of antibiotics. Even a cup of coffee can delay how fast your thyroid medicine works. The body’s digestive system is messy, unpredictable, and full of variables. That’s why adherence drops to 50% within six months for people on complex oral regimens. It’s not that they forget. It’s that the routine becomes too hard to stick to.
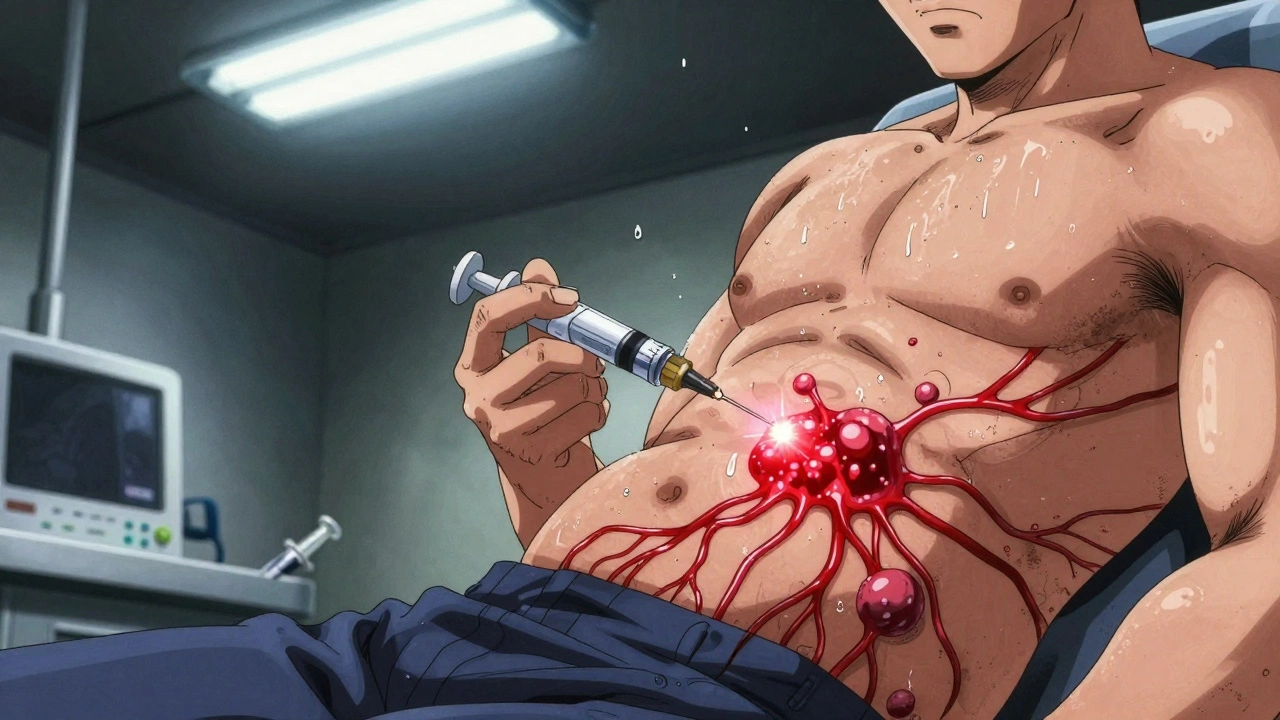
Injections: Fast, Precise, But Risky
If you need a drug to work fast-like during a heart attack, severe infection, or an allergic reaction-injections are the only real option. Intravenous (IV) drugs hit your bloodstream immediately. Peak effect? Two to five minutes. No waiting. No guesswork. That’s why hospitals use injectables for 45% of ICU medications.
But speed comes with risk. Every injection carries a chance of infection. About 1-5% of people develop redness, swelling, or even abscesses at the injection site. For people on daily insulin or biologic drugs for arthritis, that risk adds up. Long-term users often develop lipohypertrophy-fatty lumps under the skin where injections are repeated. These lumps absorb insulin poorly, leading to unpredictable blood sugar spikes.
Then there’s the psychological barrier. One in five people have needle phobia. Some avoid treatment entirely because of it. And cost? A single dose of an injectable biologic can run $2,500 to $5,000. The same drug in pill form? $25 to $100. That’s why 28% of patients on injectables stop taking them-not because they don’t work, but because they can’t afford them.
Even the way you give the shot matters. Studies show 30-40% of patients need two or three supervised sessions to learn how to inject correctly. Too shallow? The drug doesn’t absorb. Too deep? You hit a nerve or muscle. Improper technique reduces effectiveness by up to 40%. And disposal? Forty percent of patients don’t have access to sharps containers. They throw needles in the trash. That’s not just unsafe-it’s illegal.
Topical: Localized Relief, Minimal Systemic Trouble
Topical treatments-creams, gels, patches-are the quiet winners when it comes to side effects. Apply it where it hurts, and most of the drug stays right there. For skin conditions like eczema or psoriasis, topical corticosteroids are 92% less likely to suppress your adrenal glands than the same dose taken orally. That’s not a small difference. That’s life-changing for people who need long-term treatment.
Transdermal patches, like those for pain or nicotine, are designed to deliver drugs slowly through the skin into the bloodstream. They avoid the peaks and crashes of oral meds. A 2022 Mayo Clinic survey found that 74% of chronic pain patients preferred fentanyl patches over pills because they provided steady relief without drowsiness or nausea. But here’s the catch: your skin isn’t a blank slate. Damaged skin-like in psoriasis or burns-absorbs 3 to 5 times more drug than healthy skin. That means a patch that’s safe for one person could overdose another.
And application matters. Most people use too little. The standard “fingertip unit” (about 0.5 grams of ointment) is enough to cover an area the size of two adult palms. But a 2023 National Eczema Association survey found 60% of patients used less than half that amount. Result? Poor control of symptoms. Worse? They think the medication isn’t working and double up-leading to unintended systemic exposure.
Topical doesn’t mean risk-free. Skin irritation, itching, or burning at the application site happens in 15-20% of users. And some products are mislabeled. The FDA issued 23 warning letters in 2022 to companies selling creams that claimed to treat systemic conditions like high blood pressure without approval. Don’t assume “topical” means safe. Always check the label.
Why One Size Doesn’t Fit All
There’s no universal best route. It depends on what you’re treating, how fast you need results, and what your body can handle.
Oral is great for chronic conditions where steady, slow action is needed-like high blood pressure or thyroid disease. But if you have nausea from chemo, or your gut can’t absorb drugs after surgery, oral won’t cut it. That’s when injections take over.
Injectables are essential in emergencies, for patients who can’t swallow, or for drugs that break down in the stomach-like insulin or certain antibiotics. But they’re not for daily life if you can avoid them.
Topical is ideal for localized problems: joint pain, rashes, muscle soreness. It’s also the go-to for people who want to avoid stomach issues or liver stress. New tech is expanding its reach. Ultrasound-enhanced patches now let large molecules like biologics pass through skin-something once thought impossible. By 2030, experts predict a quarter of current injectables will move to advanced topical or oral forms, cutting side effects by 40-60%.
But here’s the reality: 37 critical medications still can’t be delivered any other way than by injection. Their molecules are too big, too fragile, or too unstable. Science hasn’t caught up yet. So we still need all three routes.

What Should You Do?
If you’re on a new medication, ask: Why this route? Is it because it’s the most effective-or just the most convenient? If you’re having side effects, ask if switching delivery methods could help.
For example:
- If oral NSAIDs give you stomach pain, ask about a topical gel.
- If you’re on daily insulin and hate needles, ask if an inhaled version is an option.
- If you’re using a patch and getting skin irritation, check if you’re applying it to clean, dry skin and rotating sites.
Don’t assume your doctor picked the best route just because it’s common. Ask about alternatives. Your body will thank you.
Which route of administration has the fewest side effects?
Topical administration generally has the fewest systemic side effects because the drug is designed to act locally, with minimal absorption into the bloodstream. For example, topical corticosteroids for skin conditions cause less than 5% systemic exposure compared to oral versions, which can trigger adrenal suppression, weight gain, or high blood sugar. However, topical treatments can still cause local reactions like irritation or redness at the application site.
Why do oral medications cause more stomach problems than injections?
Oral medications must pass through the digestive tract, where they can irritate the stomach lining, alter gut bacteria, or trigger nausea. Drugs like NSAIDs directly damage the protective mucus layer in the stomach, leading to ulcers in 1-2% of long-term users. Injections bypass the gut entirely, so they don’t interact with digestive enzymes or acid-making them gentler on the stomach.
Can I switch from an injection to a pill?
Sometimes, but not always. Many drugs-like insulin, certain antibiotics, or biologics for autoimmune diseases-break down in the stomach and can’t be taken orally. Others, like some painkillers or cholesterol drugs, have oral versions with similar effectiveness. Always talk to your doctor before switching. Never stop or change your route without medical advice.
Are topical creams as strong as pills?
For localized conditions like joint pain or skin inflammation, yes-they can be just as effective. But they’re not designed to treat whole-body issues like high blood pressure or infections. Topical drugs are formulated to stay on or near the skin. Even transdermal patches, which deliver drugs into the bloodstream, use much lower doses than oral or injectable versions because absorption is slow and controlled.
Why do some drugs need to be injected instead of taken orally?
Some drugs are destroyed by stomach acid or liver enzymes before they can work. Others are too large to be absorbed through the intestines-like insulin or monoclonal antibodies. Injections bypass these barriers, delivering the drug directly into the bloodstream. For drugs that need to act fast-like epinephrine during an allergic reaction-injections are the only option that works in minutes.
Is it safe to use more topical cream if it’s not working?
No. Using more than the recommended amount-like applying extra steroid cream-can lead to systemic side effects, including thinning skin, high blood pressure, or adrenal suppression. Topical doesn’t mean harmless. Always follow the dosing instructions, even if you don’t see quick results. If the medication isn’t working, talk to your doctor instead of increasing the dose.
Final Thought: Match the Route to the Need
The best delivery method isn’t the easiest one. It’s the one that gets the drug where it needs to go-with the least risk to your body. Pills are fine for daily maintenance. Shots are lifesavers in emergencies. Creams and patches offer targeted relief without flooding your system. The future of medicine isn’t about replacing one route with another. It’s about using the right tool for the job-and knowing when to choose each one.
nikki yamashita
Topical creams saved my life after years of stomach nightmares from NSAIDs. No more bloating, no more midnight runs to the bathroom. Just slap it on, feel better, and go about my day. Game changer.
Audrey Crothers
I used to hate needles so much I skipped my insulin for months 😭 Then I tried the patch-same results, zero panic. My nurse said I was ‘a poster child for transdermal’ and I’m not even mad. 💪
Robert Webb
There’s a reason we still use injections for biologics and insulin-molecular size, enzymatic degradation, bioavailability. It’s not just tradition; it’s physics and biochemistry. The gut is a brutal filter. Some molecules are just too delicate, too large, or too reactive to survive the journey through the stomach and liver. That’s why, despite all the hype around ‘needle-free’ tech, we’re still decades away from replacing half of injectables. Science doesn’t care how much we dislike needles. It cares about what works.
Nathan Fatal
People act like topical = safe. It’s not. I had a friend who used ‘extra-strength’ lidocaine cream for back pain-three times the dose-and ended up with arrhythmia. Topical doesn’t mean ‘no systemic absorption.’ It means ‘slower, but still possible.’ If you’re not monitoring dose and skin integrity, you’re gambling. And no, your ‘natural’ cream with ‘herbal extracts’ isn’t exempt from this rule.
Laura Weemering
Oral meds? The body’s equivalent of sending a letter through the postal service… except half the letters get eaten by raccoons, the rest are delayed because someone forgot to pay the postage, and then the recipient has to decipher the handwriting… and the raccoons left a mess on the doorstep. First-pass metabolism isn’t a ‘technical detail’-it’s a cosmic joke. And don’t even get me started on grapefruit juice… it’s like giving your liver a surprise party it didn’t ask for… and then the liver throws up.
wendy b
Did you know the FDA allows companies to sell topical creams labeled as ‘pain relief’ that secretly contain NSAIDs or steroids? No prescription needed. No warning labels. Just… ‘natural’ magic cream. I’ve seen people on Reddit with chemical burns from ‘herbal’ balms. The system is broken. Big Pharma doesn’t want you to know you can get the same drug in a pill for $5. They make you pay $80 for a tube that’s just a placebo with lidocaine.
Ashley Skipp
Topical is the only way to go if you don't want to be a lab rat for Big Pharma
sandeep sanigarapu
As someone from India, I see many patients avoid injections due to cost and fear. Topical options are growing, but access is unequal. In rural areas, even basic patches are unaffordable. We need policy changes, not just science. Medicine should not be a luxury.
Nathan Fatal
Robert Webb makes a great point about molecular biology-but let’s not romanticize injections. The real issue isn’t just science, it’s healthcare infrastructure. In the U.S., 1 in 4 diabetics can’t afford insulin. In developing countries, it’s worse. The delivery method is secondary to the fact that medicine is treated like a commodity, not a right. A patch won’t fix that. Policy will.