When you're going through chemotherapy, your body isn't just fighting cancer-it's also battling nausea, loss of appetite, and rapid weight loss. It’s not about eating healthy in the usual sense. It’s about eating enough to keep your strength up, your immune system working, and your treatment on track. Many people assume they should eat light or skip meals when they feel sick. That’s the opposite of what you need. Chemotherapy nutrition isn’t a suggestion-it’s a medical necessity.
Why Normal Diet Rules Don’t Apply During Chemotherapy
If you’ve ever followed a weight-loss plan or tried to eat clean, you’ve probably been told to avoid sugar, cut carbs, and go easy on fats. During chemotherapy, those rules can hurt you. Your body needs more calories and protein than ever before. The standard recommendation for a healthy adult is 0.8 grams of protein per kilogram of body weight. For someone on chemo, that number jumps to 1.2 to 2.0 grams per kilogram. That’s nearly double. And your calorie needs? They go up by 20-30%. If you weighed 70 kg before treatment, you’re now looking at 2,100-2,500 calories a day just to stay even. This isn’t about vanity. It’s about survival. When your body doesn’t get enough fuel, it starts breaking down muscle-your heart, lungs, and immune system all suffer. Studies show that patients who lose weight during treatment are more likely to need dose reductions or delays. That means less effective therapy and longer recovery. The European Society for Clinical Nutrition and Metabolism (ESPEN) says outright: don’t restrict calories if you’re losing weight. That’s not a suggestion. That’s a rule.Taming Nausea: What to Eat and What to Avoid
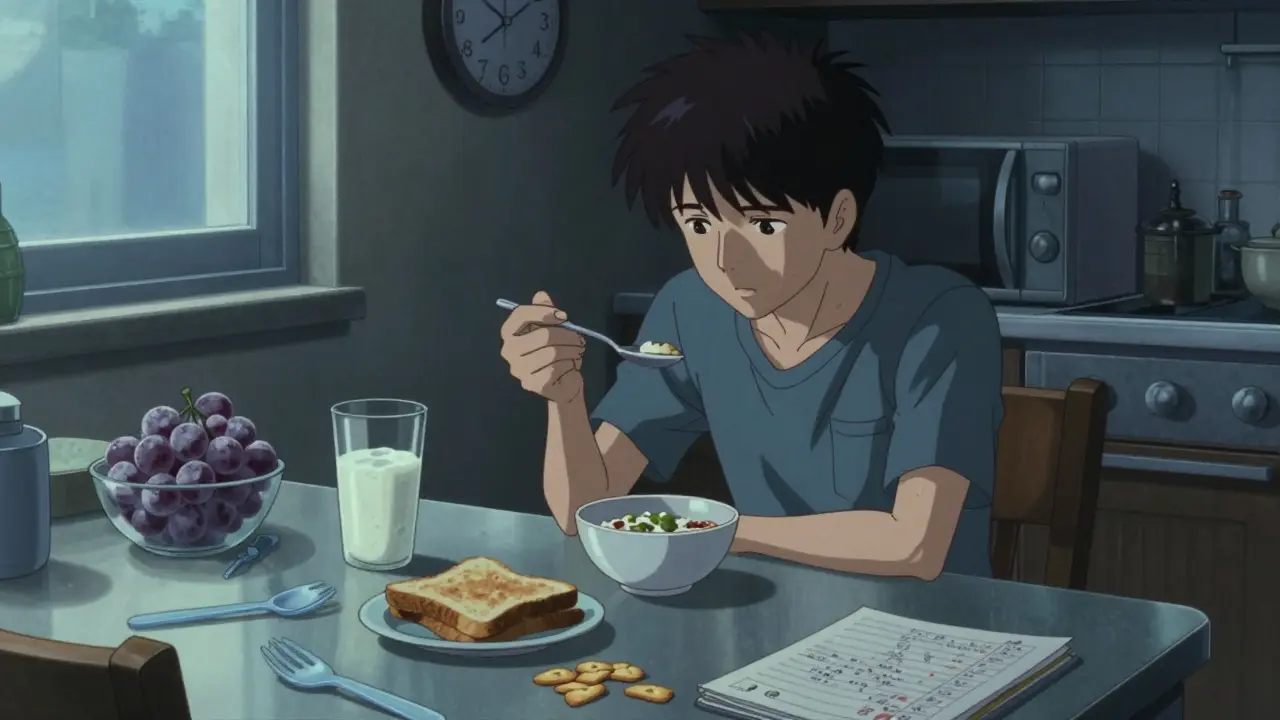
Nausea is one of the most common and crushing side effects of chemotherapy. It’s not just feeling a little queasy-it can make you dread every meal. The good news? There are proven ways to fight it. First, ditch greasy, fried, or overly rich foods. These trigger nausea in 73% of patients, according to the Academy of Nutrition and Dietetics. Think burgers, fried chicken, creamy sauces. Instead, go for bland, dry, or cool foods. Crackers, toast, rice, and plain pasta are your friends. Cold foods often work better than hot ones because they don’t release strong smells. Try chilled watermelon, yogurt, or a smoothie straight from the fridge. Drink fluids between meals, not with them. Sipping water or ginger tea during meals fills your stomach too fast, making nausea worse. Wait 30 minutes after eating to drink. And keep sipping all day. Dehydration makes nausea worse and can lead to fatigue and dizziness. Strong smells are another trigger. If the smell of coffee or garlic makes you gag, avoid it. Use plastic utensils instead of metal-many patients say metal gives food a bitter, unpleasant taste. Keep your kitchen well-ventilated. Cook in small batches or use a microwave to limit odor spread. Ginger is a real winner. Ginger chews, ginger tea, or even ginger ale (the kind with real ginger) help reduce nausea in many patients. One study found that 68% of people using ginger reported less vomiting and more ability to eat. Keep a pack of ginger chews in your bag or by your bed.Small Meals, Big Results
Forget three big meals a day. That’s too much for a stomach that’s already under stress. Instead, eat five to six small meals every 2-3 hours. Each should have 300-400 calories and at least 20-30 grams of protein. That’s the sweet spot. Think of it like refueling a car-not filling the tank all at once. You’ll feel less bloated, less nauseous, and more in control. And you’ll get more total calories and protein over the day. Here’s what a day might look like:- 7:00 AM: 1 cup Greek yogurt with 2 tablespoons peanut butter and a banana
- 10:00 AM: 2 hard-boiled eggs and a slice of white toast with honey
- 1:00 PM: Chicken and rice soup with a handful of crackers
- 4:00 PM: Protein shake made with full-fat milk, banana, and a scoop of whey or plant-based protein
- 7:00 PM: Scrambled eggs with cheese and mashed potatoes
- 9:30 PM: Cottage cheese with a few pineapple chunks

Protein Is Your Lifeline
You need protein to repair tissues, fight infection, and keep your muscles from melting away. But most people don’t know how much they really need. A 150-pound person on chemo needs at least 70 grams of protein a day. That’s 3-4 times more than the average person gets from a single chicken breast. Good protein sources that are easy to tolerate:- Eggs (cooked fully-no runny yolks)
- Greek yogurt (full-fat for extra calories)
- Cottage cheese
- Peanut butter
- Chicken, turkey, or fish (cooked well)
- Protein shakes or powders (look for ones with 20g+ per serving)
- Smoothies with milk, nut butter, and fruit
Food Safety: Don’t Risk Infection
Chemotherapy weakens your immune system. That means foods that are safe for healthy people can be dangerous for you. Raw or undercooked meat, fish, and eggs are off-limits. Even a little Salmonella can land you in the hospital. Follow these rules:- Never eat raw oysters, sushi, or rare steak
- Cook eggs until the yolk is solid (160°F or 71°C)
- Avoid homemade mayonnaise, Caesar dressing, or cookie dough with raw eggs
- Wash all produce thoroughly
- Reheat leftovers until steaming hot
- Use clean utensils and wash hands before eating
Real People, Real Solutions
You’re not alone in this. Thousands of patients have walked this path and found ways to make it work. - Freeze grapes. They’re cold, sweet, and gentle on sore mouths. A top tip from 89 people on the CancerCare forum. - Keep snacks visible. Put trail mix, cheese sticks, or protein bars on your kitchen counter, nightstand, and car. Out of sight = out of mind. You’re more likely to eat if it’s right there. - Use plastic utensils. Metal tastes metallic to many patients. Plastic eliminates that bitter aftertaste. - Make protein shakes at home. Store-bought options like Ensure Plus cost $35-$45 for a 12-pack. A homemade version with yogurt, peanut butter, and milk costs under $2 per serving. One Reddit user shared that after two weeks of drinking three homemade shakes a day, she gained 4 pounds-something she hadn’t done in months. She said it was the first time she felt like she was winning.
When Food Isn’t Enough
Sometimes, even the best plan falls short. If you’re losing weight despite trying everything, or if you can’t keep anything down for days, talk to your care team. You might need help beyond food. Oral nutrition supplements like Juven (a medical food with HMB) are designed for muscle loss in cancer patients. They’re covered by some insurance plans. If cost is an issue, ask your hospital’s social worker. Many centers offer free or discounted supplements. In more severe cases, tube feeding or IV nutrition may be needed. This isn’t failure-it’s support. About 15-20% of patients on aggressive chemo regimens need this. It’s not about giving up. It’s about giving your body what it needs to keep going.What’s Changing Now
The field of oncology nutrition is growing fast. In 2023, the National Cancer Institute launched a free mobile app called “Nutrition During Treatment.” It tracks calories, protein, nausea levels, and even suggests recipes based on your symptoms. Over 42,000 people downloaded it in six months. Hospitals are catching on too. Mayo Clinic’s standardized nutrition program cut treatment delays due to malnutrition by 28% in just one year. And research is moving toward personalized nutrition-using your genes to figure out what foods help you most. The message is clear: nutrition isn’t a side note in cancer care. It’s part of the treatment.Final Thoughts: Eat Like Your Life Depends on It-Because It Does
This isn’t about eating for health. It’s about eating to survive. You’re not trying to lose weight or get lean. You’re trying to stay strong enough to finish treatment. Every bite counts. Start today. Set alarms for meals. Keep snacks nearby. Drink your protein. Avoid triggers. And if you’re struggling, ask for help. Oncology dietitians exist for this exact reason. They’re not luxury add-ons-they’re essential members of your care team. You’re fighting cancer. Don’t let hunger be your second battle. Fuel your body. It’s the most powerful medicine you have left.How much protein do I need during chemotherapy?
You need 1.2 to 2.0 grams of protein per kilogram of body weight daily. For a 70 kg person, that’s 84 to 140 grams of protein each day-nearly double what a healthy adult needs. This helps prevent muscle loss and supports healing. Use high-protein foods like Greek yogurt, eggs, peanut butter, and protein shakes to reach this goal.
Should I eat three big meals or small meals often?
Eat five to six small meals every 2-3 hours. Large meals can worsen nausea and make you feel bloated. Small meals help you get more calories and protein without overwhelming your stomach. Each meal should have 300-400 calories and at least 20-30 grams of protein.
What foods make nausea worse during chemotherapy?
Greasy, fried, and high-fat foods make nausea worse in 73% of patients. Strong-smelling foods like garlic, onions, or coffee can also trigger it. Avoid spicy foods if your mouth is sore. Cold, bland foods like toast, crackers, rice, and chilled yogurt are easier to tolerate.
Is it safe to drink protein shakes during chemo?
Yes, protein shakes are not only safe but often essential. Homemade shakes with full-fat yogurt, peanut butter, milk, and fruit are cost-effective and nutrient-dense. Avoid raw eggs or unpasteurized ingredients. Store-bought shakes like Ensure Plus are fine, but homemade versions can be just as good and cheaper.
Can I eat raw fruits and vegetables during chemotherapy?
Wash them thoroughly, but avoid raw sprouts, unpeeled fruits, and unwashed produce. Your immune system is weakened, so bacteria from raw foods can cause serious infections. Peel fruits like apples and bananas. Cook vegetables when possible. If you eat raw, choose firm, non-blemished produce and rinse under running water.
What if I can’t eat anything for days?
Contact your care team immediately. Going without food for more than 2-3 days can lead to dangerous weight loss and dehydration. Your doctor may recommend oral nutrition supplements, tube feeding, or IV nutrition. These are not signs of failure-they’re tools to keep you strong enough to finish treatment.
Are there free or low-cost nutrition resources available?
Yes. The American Cancer Society offers a free 24/7 helpline and connects patients with local nutrition services through their Road to Recovery program. Many hospitals have dietitians who work with patients at no extra cost. Some programs provide free protein shakes or supplements to those who qualify. Ask your oncology nurse or social worker-they know what’s available.
Cassie Widders
Just ate a spoonful of peanut butter straight from the jar at 3 AM. Felt like a win. No fancy recipes, no guilt. Just fuel.
Ben Kono
I stopped eating solid food for five days and just drank protein shakes with whole milk and honey my wife made me and somehow gained three pounds I didn’t think was possible
Darryl Perry
While the general advice is sound the lack of citation for the 73% nausea statistic is concerning. The Academy of Nutrition and Dietetics does not publish such granular data in publicly accessible peer-reviewed sources. This undermines credibility.
Windie Wilson
So let me get this straight you’re telling me to eat like a bear pre-hibernation but avoid anything that tastes like food? Also why is everyone suddenly obsessed with peanut butter is this a cult or just chemo brain
Rinky Tandon
As a certified oncology nutritionist with over 12 years of clinical experience in Mumbai I can unequivocally state that the protein thresholds cited here are grossly insufficient for Indian patients undergoing platinum-based regimens. The ESPEN guidelines are Western-centric and fail to account for baseline sarcopenia in South Asian populations. You need at least 2.2g/kg for those under 60 with BMI under 19. And no ginger tea is useless if your gut flora is destroyed by prior antibiotics. Try curcumin-infused lassi with full-fat yogurt and jaggery. That’s evidence-based Ayurvedic oncology nutrition. Also stop using plastic utensils-metal is fine if you rinse it with chlorhexidine. You’re overreacting to phantom tastes.
Konika Choudhury
Why are we listening to Americans when our grandmothers knew how to feed sick people better than any hospital dietitian ever did My mother gave me boiled rice with ghee and a pinch of salt when my uncle was in chemo and he lived three years longer than his prognosis said he would You don’t need protein shakes you need real food made with love
Daniel Pate
It’s interesting how we frame nutrition as a weapon against cancer when in reality it’s just a buffer. The body doesn’t care if you eat 2500 calories or 1800 it just wants to survive. The real question is whether the chemo protocol itself is compatible with metabolic resilience. Maybe we’re putting the cart before the horse. What if the problem isn’t what you eat but what the drugs do to your mitochondria
Alex Fortwengler
Anyone else notice that every single food recommendation here is either peanut butter or yogurt What if I’m lactose intolerant and allergic to peanuts What if I’m vegan What if I just can’t stand the taste of anything after chemo What if this whole thing is just Big Pharma pushing protein powder sales disguised as medical advice
jordan shiyangeni
It is deeply troubling that this article casually recommends consuming high-fat dairy products without addressing the well-documented link between saturated fat intake and increased systemic inflammation in cancer patients. Furthermore, the endorsement of homemade protein shakes using whole milk and peanut butter is not only nutritionally unsound but potentially hazardous given the high caloric density and glycemic load of such formulations. One must consider the insulin-like growth factor-1 (IGF-1) axis, which is known to promote tumor proliferation. The notion that more calories equate to better outcomes is a dangerous oversimplification rooted in outdated nutritional dogma. The body does not need fuel-it needs bioavailable micronutrients and anti-inflammatory phytochemicals. Recommend cruciferous vegetable extracts and omega-3 supplementation from algae oil instead. This is not merely dietary advice-it is a matter of oncological ethics.
steve ker
Protein shakes are overrated. Just eat eggs. Real ones. Not that fake stuff. Done.