NSAID Risk Assessment Tool
This tool helps you assess your personal risk of gastrointestinal bleeding from NSAID use based on key medical factors. Select the risk factors that apply to you to see your risk level and get personalized recommendations.
Your Risk Assessment
Your risk level is low. Continue taking NSAIDs as prescribed and monitor for symptoms. Consult your doctor if you experience black stools, vomiting blood, or unexplained fatigue.
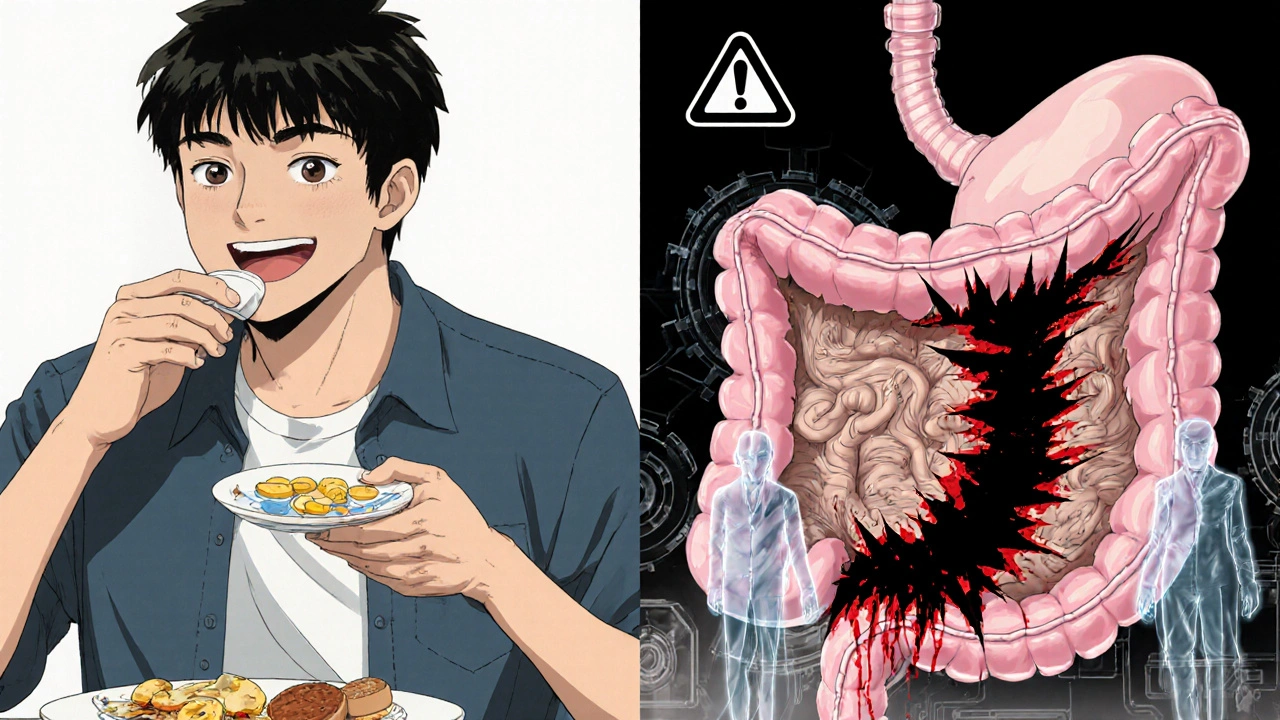
Every year, millions of people reach for ibuprofen, naproxen, or diclofenac to ease a headache, sore knee, or back pain. These are NSAIDs-non-steroidal anti-inflammatory drugs-and they work. But for many, they also quietly damage the stomach lining, leading to bleeding that can be life-threatening. The problem isn’t rare. It’s hidden. And it’s growing.
How NSAIDs Hurt Your Stomach
NSAIDs block enzymes called COX-1 and COX-2. COX-2 causes pain and swelling, so blocking it helps. But COX-1 protects your stomach lining by making mucus and keeping blood flowing to the gut. When NSAIDs shut down COX-1, your stomach loses its natural shield. Even a single dose can start the damage. Over time, it leads to erosions, ulcers, and bleeding.
It doesn’t take a big dose. A 2021 review in Clinics in Medicine found that 26% of people take over-the-counter NSAIDs at doses higher than recommended-and most never tell their doctor. The damage isn’t always obvious. Some people get black, tarry stools (melena). Others feel tired and pale from slow, silent bleeding that drains iron over months. One study showed 86% of patients with lower GI bleeding had taken NSAIDs, even without a peptic ulcer.
Who’s at the Highest Risk?
Not everyone who takes NSAIDs bleeds. But some people are far more vulnerable. Experts have identified clear risk factors:
- Age over 65-your stomach lining thins with time
- History of peptic ulcer or GI bleeding-once it happens, it’s more likely to happen again
- Taking blood thinners like warfarin or aspirin-this doubles the chance of serious bleeding
- Using corticosteroids like prednisone-these weaken the gut lining too
- Taking more than one NSAID at once-combining ibuprofen and naproxen doesn’t help pain, it multiplies risk
- Chronic conditions like heart failure or kidney disease-these make your body less able to repair damage
Doctors use a simple scoring system to measure risk: age over 70 (2 points), past ulcer (2 points), blood thinners (2 points), steroids (1 point). If your score is 2 or higher, you’re in the high-risk group. And if you’re high risk, you shouldn’t be taking NSAIDs without protection.
COX-2 Inhibitors: Safer for the Stomach, Riskier for the Heart
For years, drugs like celecoxib (Celebrex) and rofecoxib (Vioxx) were marketed as stomach-friendly NSAIDs. They only block COX-2, leaving COX-1 alone. A 2000 Lancet study found celecoxib cut serious ulcers by half compared to ibuprofen.
But there’s a catch. Blocking COX-2 too much raises the risk of heart attacks and strokes. Rofecoxib was pulled from the market in 2004 after the APPROVe trial showed it doubled heart attack risk. Celecoxib is still around, but it carries a black box warning from the FDA for cardiovascular danger.
So it’s not about picking the “safest” NSAID. It’s about matching the drug to the person. For someone with arthritis and a history of ulcers but no heart disease, a COX-2 inhibitor with a proton pump inhibitor (PPI) may be the best choice. For someone with heart disease and no GI history, even a COX-2 inhibitor might be too risky.
Protection: PPIs and Misoprostol
If you need NSAIDs and you’re high risk, you need a shield. The strongest shield is a proton pump inhibitor-drugs like omeprazole, esomeprazole, or pantoprazole. A 2017 Cochrane review of over 13,000 patients found PPIs reduce NSAID-related ulcers and bleeding by 75%.
Another option is misoprostol, a drug that replaces the protective mucus NSAIDs destroy. It works almost as well as PPIs-but it causes diarrhea in 1 in 5 people and cramping in 1 in 8. That’s why most doctors choose PPIs instead.
Now there’s a new option: Vimovo. It’s a single pill that combines naproxen with esomeprazole. In the 2022 PRECISION-2 trial, people taking Vimovo had a 7.3% chance of ulcer complications. Those taking naproxen alone? 25.6%. That’s a 72% drop in risk.
Real Stories Behind the Numbers
Behind every statistic is a person. On Reddit’s r/geriatrics, a user shared how their 78-year-old mother needed three blood transfusions after months of unexplained fatigue. She’d been taking ibuprofen daily for arthritis. No one connected the dots until her hemoglobin dropped to 6.8-half the normal level.
On HealthUnlocked, 63% of 247 people reported stomach pain, nausea, or dark stools from NSAIDs-but only 37% told their doctor. Many assumed it was just “indigestion.” Others didn’t want to stop their pain relief.
And then there’s the flip side. On Drugs.com, 78% of people who took celecoxib said it worked well with no stomach issues. But 42% of arthritis patients surveyed by the Arthritis Foundation quit NSAIDs altogether because of GI symptoms. That’s not just discomfort-it’s a loss of quality of life.

What You Should Do
If you’re taking NSAIDs regularly, here’s what to do:
- Ask yourself: Do I really need this? Can I use heat, physical therapy, or acetaminophen instead?
- If you’re over 65, have had an ulcer, or take blood thinners, talk to your doctor about switching to a COX-2 inhibitor with a PPI.
- Don’t combine NSAIDs. Never take ibuprofen and naproxen together. Even one daily aspirin can add to the risk.
- Watch for warning signs: black stools, vomiting blood, sudden weakness, or unexplained fatigue. These aren’t normal.
- If you’ve been on NSAIDs for more than a few weeks, ask for a blood test to check for anemia. Iron deficiency is often the first clue.
The American College of Gastroenterology says for people with prior bleeding, COX-2 inhibitors plus PPI reduce complications by 80%. The number needed to treat? Just 16 people to prevent one serious event in 12 weeks.
The Bigger Picture
NSAID-related GI bleeding causes 107,000 hospitalizations and 16,500 deaths every year in the U.S. alone. The cost? Over $2 billion. Yet these drugs are still the go-to for pain because they work fast and cheap.
The future may hold safer options. New drugs called CINODs-like naproxcinod-are in trials. They release nitric oxide, which helps protect the gut while still blocking pain. Early results show 50% fewer ulcers than naproxen.
But for now, the answer isn’t a new drug. It’s awareness. It’s asking questions. It’s knowing that your daily pain pill isn’t harmless. It’s a tool-and like any tool, it can cut both ways.
Can I take ibuprofen if I’ve had a stomach ulcer before?
No. If you’ve had a peptic ulcer or GI bleeding, taking ibuprofen or other non-selective NSAIDs greatly increases your risk of another bleed. The American College of Gastroenterology recommends using a COX-2 inhibitor like celecoxib with a proton pump inhibitor (PPI) instead. Even then, you should only use the lowest effective dose for the shortest time possible.
Are over-the-counter NSAIDs safer than prescription ones?
No. The risk of gastrointestinal bleeding comes from the drug itself, not whether it’s prescription or OTC. Ibuprofen and naproxen sold without a prescription are the same chemicals as the prescription versions. The difference is dose and duration. Many people take OTC NSAIDs daily for months without realizing they’re at risk. The FDA requires all NSAIDs to carry black box warnings about GI bleeding, regardless of how they’re sold.
Does taking NSAIDs with food prevent stomach bleeding?
Taking NSAIDs with food may reduce mild irritation or heartburn, but it doesn’t prevent ulcers or serious bleeding. The damage happens at the cellular level-NSAIDs block protective enzymes in the stomach lining. Food doesn’t stop that. If you’re at risk, you need a proton pump inhibitor (PPI) or misoprostol, not just a sandwich.
How long does it take for NSAIDs to cause bleeding?
Bleeding can happen anytime-from the first dose to after years of use. Some people develop ulcers within days, especially if they’re high risk. Others have slow, hidden bleeding that leads to anemia over months. That’s why regular blood tests are important if you’re on long-term NSAIDs. Don’t wait for black stools or vomiting blood-by then, it’s often too late.
Can I stop NSAIDs cold turkey if I’m worried about bleeding?
If you’re taking NSAIDs for chronic pain like arthritis, stopping suddenly can cause a flare-up. Don’t quit without talking to your doctor. Instead, ask about alternatives: physical therapy, acetaminophen, topical pain relievers, or a safer NSAID combo like a COX-2 inhibitor with a PPI. Your doctor can help you switch safely while managing your pain.
Is it safe to take a daily low-dose aspirin with an NSAID?
No. Aspirin is an NSAID too, and it blocks COX-1 just like ibuprofen or naproxen. Taking it with another NSAID doubles your risk of bleeding. If you’re on aspirin for heart protection and need pain relief, talk to your doctor about alternatives. Acetaminophen is often the safest choice. If you must use an NSAID, you’ll likely need a proton pump inhibitor (PPI) to protect your stomach.

Margo Utomo
Seriously? People still take ibuprofen like it's candy? 😅 I had a friend bleed out from a silent ulcer after 3 years of 'just a little for my back'. PPIs aren't optional if you're on NSAIDs long-term. Your stomach isn't a backup battery.
mike tallent
This is such an important post. 🙌 I'm a PT and see this all the time - older folks with arthritis who’ve been on naproxen since 2010 and think 'it's just gas'. Blood tests for iron should be standard every 6 months for anyone on chronic NSAIDs. Seriously, folks - get checked.
Deepali Singh
The 72% reduction with Vimovo is statistically significant but clinically misleading. The trial excluded patients with CVD. Real-world adherence to PPIs is under 40%. This data doesn't reflect the chaos of polypharmacy in elderly populations. Also, cost is prohibitive for most.
Matt Wells
It is, indeed, a regrettable epistemological failure of public health literacy that non-prescription NSAIDs are perceived as benign. The pharmacodynamic inhibition of COX-1 is not mitigated by ingestion with food, nor is it rendered less hazardous by virtue of over-the-counter status. The FDA black box warning is not a suggestion.
jalyssa chea
why do doctors even prescribe this stuff anymore i mean like i get it pain sucks but like why not just give people yoga or something idk i feel like we overmedicate everything and then act shocked when people get sick
Joyce Genon
Let’s be real - the entire NSAID industry is a scam. PPIs are more profitable than the drugs themselves. Big Pharma doesn’t care if you bleed - they just want you to keep buying the next pill. And don’t even get me started on celecoxib. It’s just a heart attack waiting to happen with a side of indigestion. The real solution? Stop taking everything. Fast. Always.
Abdul Mubeen
I wonder if this is all a government ploy to push PPI sales. Did you know that the Cochrane review was funded by AstraZeneca? And why is Vimovo only available in the US? Why not the UK? There’s a pattern here. NSAIDs are safe. The real danger is trusting pharmaceutical marketing.
Jennifer Howard
I cannot believe people are still being so irresponsible. If you are taking NSAIDs without a PPI and you are over 50, you are essentially playing Russian roulette with your gastrointestinal tract. There is no excuse. Not for arthritis. Not for headaches. Not for 'it just feels better'. You are not special. You are not immune. You are statistically doomed.
Julie Roe
I’ve been helping my mom manage her knee pain for years, and this post hit home. She was on naproxen for 8 years - no idea she was bleeding internally. We switched to acetaminophen + physical therapy + a PPI. Her energy came back. Her color improved. She stopped feeling like a ghost. It’s not about giving up pain relief - it’s about finding safer ways to live with it. You don’t have to suffer silently. Ask for help. You deserve to feel better without risking your life.
Gary Lam
In my family, we say 'if it hurts, take a nap, not a pill'. 🇺🇸🇨🇳 My dad took ibuprofen for 20 years, thought he was fine. Got admitted for a GI bleed on his 72nd birthday. Now he drinks turmeric tea and does tai chi. Still complains about his knees… but he’s alive. And he’s got his dignity. That’s worth more than a quick fix.
Eva Vega
The pharmacokinetic profile of COX-2 selective inhibitors demonstrates a significantly reduced incidence of upper GI mucosal injury compared to non-selective NSAIDs, as validated by endoscopic studies. However, the concomitant use of PPIs remains a cornerstone of risk mitigation in high-risk cohorts per ACG guidelines. The pharmacoeconomic burden of NSAID-related complications necessitates a tiered therapeutic algorithm.
John Wayne
Funny how everyone acts like NSAIDs are the enemy. You know what else causes GI bleeds? Stress. Coffee. Alcohol. Smoking. But no one blames those. It’s always the pill. The real issue? People don’t take responsibility for their own health. They want a magic bullet. There isn’t one. Stop blaming drugs. Start blaming your lifestyle.
George Gaitara
I’m just saying - what if the real problem isn’t NSAIDs? What if it’s that we’re all just too damn sedentary? We sit all day, then we take pills to fix the pain from sitting, then we take more pills to fix the damage from the first pills. It’s a pyramid scheme of suffering. And the doctors? They’re just the middlemen. We’re all just rats on a wheel.
Sylvia Clarke
I love how this post doesn’t just throw facts at us - it tells stories. The 78-year-old woman with the hemoglobin of 6.8? That’s not a statistic. That’s someone’s mom. That’s someone’s grandma. That’s someone’s future if we keep ignoring this. And yet, we still swipe ibuprofen like it’s gum. We’ve turned medicine into a convenience store. But your stomach doesn’t care if you’re in a hurry. It just wants to survive. So maybe… just maybe… pause before you pop that pill.