If you're taking ledipasvir, you're likely doing so because you're treating hepatitis C. That’s a good thing - it’s one of the most effective treatments available. But like any medicine, it comes with risks. You might have heard stories about side effects, or maybe your doctor mentioned a few warning signs. What you need to know isn’t just what can go wrong - it’s what to watch for, when to act, and how to stay safe while your body clears the virus.
What Ledipasvir Actually Does
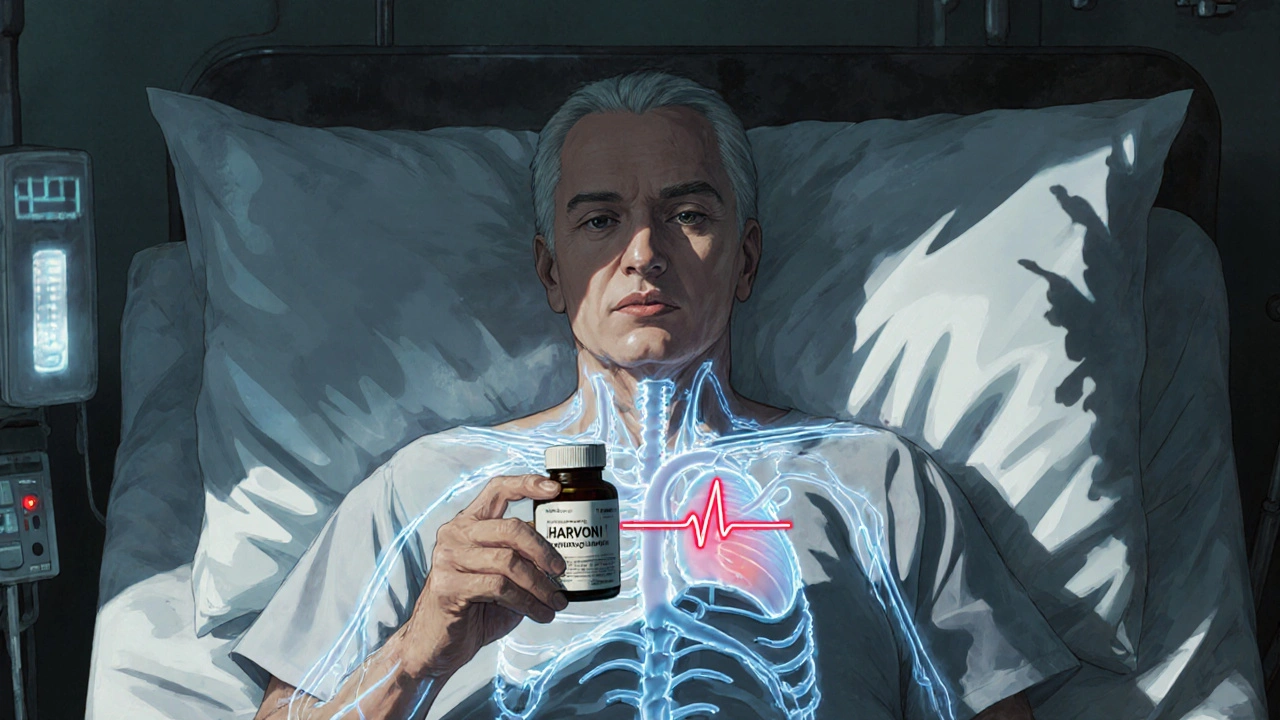
Ledipasvir is not a standalone drug. It’s always paired with sofosbuvir in a single pill called Harvoni. Together, they block the hepatitis C virus from multiplying. This combo works against genotype 1, the most common strain in the U.S., Australia, and Europe. Clinical trials showed over 95% of patients cleared the virus after 8 to 12 weeks. That’s not just effective - it’s life-changing. But effectiveness doesn’t mean safety for everyone.
Common Side Effects You Might Notice
Most people tolerate ledipasvir well. But about 1 in 5 will feel something off. These aren’t rare - they’re expected. The most common issues include:
- Fatigue - feeling worn out even after a full night’s sleep
- Headaches - usually mild, not migraine-level
- Nausea - sometimes just a queasy feeling, rarely vomiting
- Weakness - not muscle loss, but a general lack of energy
- Diarrhea - occasional, not chronic
These don’t mean the drug is failing. They mean your body is reacting. Most fade after the first two weeks. If fatigue hits hard, try napping in the afternoon. If nausea sticks around, eat small, bland meals - crackers, rice, toast. Don’t push through it. Your liver is already under stress. Don’t add more strain.
Serious Side Effects - When to Call Your Doctor
These are rare, but they’re serious. You need to recognize them fast.
- Slow heartbeat (bradycardia) - especially if you’re also taking amiodarone. This combo can cause your heart to drop to dangerously low rates. It’s been linked to cardiac arrest in some cases. If you feel dizzy, faint, or your chest feels like it’s skipping beats, stop taking it and get help immediately.
- Severe liver damage - if you have advanced cirrhosis, ledipasvir can trigger a sudden drop in liver function. Signs: yellowing skin or eyes, dark urine, swelling in your legs, confusion. This isn’t a wait-and-see situation. Go to the ER.
- Allergic reactions - rash, itching, swelling of the face or throat, trouble breathing. Even if it seems mild at first, it can escalate fast.
One patient in Sydney, 58, started Harvoni in January 2024. Two weeks in, he noticed his hands were trembling and he couldn’t climb stairs without stopping. His doctor checked his heart rate - 42 beats per minute. He’d been on amiodarone for atrial fibrillation. That combo was the cause. He stopped both drugs, switched to a safer regimen, and cleared the virus without incident.
Drug Interactions - The Hidden Danger
Ledipasvir doesn’t just talk to your liver. It talks to your entire system. The biggest red flag? Amiodarone. This heart rhythm drug is common in older adults. Taking it with ledipasvir is dangerous. The FDA issued a black box warning in 2016. Don’t take them together unless you’re under strict monitoring in a hospital.
Other risky drugs include:
- Statins like simvastatin - can raise muscle damage risk
- Some HIV meds like tenofovir alafenamide - can increase kidney stress
- St. John’s wort - makes ledipasvir less effective
- Antacids with aluminum or magnesium - if taken too close, they block absorption
If you take any of these, your doctor needs to know. Even over-the-counter stuff. Don’t assume it’s harmless. A simple antacid taken two hours before your pill can cut absorption by 50%.
Precautions Before You Start
Before you swallow that first pill, make sure these boxes are checked.
- Get a full liver panel - including albumin, bilirubin, and INR. If your liver is already failing, ledipasvir might not be the right choice.
- Review every medication - including supplements, vitamins, and herbal teas. Write them down. Bring the list to your appointment.
- Test for hepatitis B - if you’ve had it in the past, ledipasvir can reactivate it. You’ll need to be on antivirals for HBV too.
- Check kidney function - if your eGFR is below 30, your dose may need adjusting.
- Don’t drink alcohol - even one drink a week can speed up liver damage. You’re trying to heal your liver. Don’t sabotage it.
One woman in Melbourne, 62, skipped the hepatitis B test. She’d had it as a teenager and thought she was fine. Two weeks into treatment, her liver enzymes spiked. She ended up in the hospital with reactivated HBV. A simple blood test could’ve prevented it.
Special Populations - Who Needs Extra Care
Not everyone responds the same way.
- Pregnant women - ledipasvir hasn’t been tested in pregnancy. If you’re pregnant or planning to be, talk to your doctor. Hepatitis C can pass to the baby, but so can the risks of treatment.
- People over 65 - older adults are more likely to have other health issues and take more meds. More interactions. More risk.
- People with kidney disease - ledipasvir is cleared by the liver, but the combo pill includes sofosbuvir, which can affect kidneys. Monitor eGFR monthly.
- Those with HIV co-infection - you can take ledipasvir, but you need to be on stable HIV meds. Some HIV drugs clash with it.
What to Do If You Miss a Dose
Take it as soon as you remember - unless it’s almost time for your next dose. Then skip the missed one. Don’t double up. Missing one dose won’t ruin your cure rate. But taking two at once can raise your risk of side effects. Consistency matters more than perfection.
After Treatment - What Comes Next
Even after you finish the 8- to 12-week course, you’re not done. You need a follow-up blood test 12 weeks later. That’s when they check for sustained virologic response - SVR12. If the virus is gone, you’re cured. But your liver still needs care.
Stop alcohol. Eat well. Get vaccinated for hepatitis A and B if you haven’t already. Keep your weight in check. Your liver is healing, but it’s still vulnerable.
Bottom Line
Ledipasvir is one of the best tools we have to beat hepatitis C. But it’s not a magic pill. It’s a powerful tool that needs respect. Know the side effects. Know the interactions. Know your own health history. Talk to your doctor. Don’t assume it’s safe just because it’s widely prescribed. Your body is unique. Your treatment should be too.
Can ledipasvir cause liver damage?
Yes - but only in rare cases, mostly in people with advanced cirrhosis. Ledipasvir itself doesn’t damage the liver. But if your liver is already severely scarred, clearing the virus too quickly can cause inflammation and a sudden drop in function. This is called hepatic decompensation. Signs include jaundice, swelling, confusion, or bleeding. If you have cirrhosis, your doctor will monitor you closely during and after treatment.
Is it safe to take ledipasvir with amiodarone?
No. The combination can cause a dangerous slowing of the heart rate, even leading to cardiac arrest. The FDA warns against using them together. If you’re on amiodarone for heart rhythm issues, your doctor must switch you to a different heart medication before starting ledipasvir. Never combine them without medical supervision.
Can I drink alcohol while taking ledipasvir?
No. Alcohol puts extra stress on your liver - the same organ you’re trying to heal. Even moderate drinking can increase scarring and reduce your chances of a full cure. If you’ve been drinking regularly, talk to your doctor before starting treatment. You may need support to stop safely.
How long do side effects last?
Most common side effects - fatigue, headache, nausea - peak in the first two weeks and fade as your body adjusts. By week 4, most people feel back to normal. If side effects get worse after the first month, or if new ones appear, contact your doctor. It could signal a drug interaction or another health issue.
Do I need blood tests while on ledipasvir?
Yes. Before starting, you’ll need tests for liver function, kidney function, hepatitis B status, and HIV. During treatment, your doctor will likely check liver enzymes at week 4 and again at the end. After finishing, you’ll need an SVR12 test - a blood test 12 weeks later - to confirm the virus is gone. These aren’t optional. They’re essential for safety and success.
What to Do Next
If you’re starting ledipasvir, make a checklist: write down every medication you take, schedule your baseline blood tests, and ask your doctor about hepatitis B. If you’re already on it, keep track of how you feel each day. Note any new symptoms. Don’t ignore fatigue or dizziness - they’re signals, not inconveniences. Your goal isn’t just to finish the pills. It’s to finish cured - and stay that way.
Dion Hetemi
Bro, I took Harvoni last year and honestly? The fatigue was brutal. I thought I was just lazy, but nope - my body was fighting a war inside. I napped like a damn toddler and still felt like I’d run a marathon. But hey - 12 weeks later, virus gone. Worth every second of zombie mode. Don’t let the side effects scare you off - just pace yourself.
Kara Binning
Amiodarone and ledipasvir? That’s a death sentence waiting to happen. I saw a guy in the ER last year - 67, on both, went into full cardiac arrest. They had to shock him twice. The FDA warning? It’s not a suggestion. It’s a lifeline. If your cardiologist prescribes this combo, find a new doctor. ASAP.
river weiss
It is imperative to underscore that the concomitant use of ledipasvir with amiodarone constitutes a contraindication of the highest order. Moreover, the potential for hepatic decompensation in patients with advanced cirrhosis is not merely theoretical - it is empirically documented in multiple peer-reviewed studies. Furthermore, the pharmacokinetic interference caused by aluminum- or magnesium-containing antacids is well-established and necessitates a minimum two-hour separation from dosing. These are not minor considerations; they are non-negotiable components of safe administration.
Brian Rono
Let’s be real - this whole ‘ledipasvir is a miracle drug’ narrative is corporate propaganda dressed in white coats. Sure, it cures HCV - but at what cost? Fatigue? Nausea? Heart arrhythmias? People are dying because doctors treat this like a pharmacy checklist instead of a biological minefield. And don’t even get me started on the ‘just avoid alcohol’ advice - like we’re all 18-year-olds who drink beer on weekends. Some of us have been drinking since high school. You think a ‘no alcohol’ sign is gonna stop a 55-year-old with cirrhosis? Please. This isn’t medicine - it’s moralizing with a prescription pad.
Zac Gray
Look, I get it - you’re trying to heal. But let’s not pretend this is a spa day. You’re not just taking a pill; you’re letting a biochemical scalpel cut through your liver’s worst enemy - and yes, that’s gonna rattle your whole system. The fatigue? It’s your body rebuilding. The nausea? Your liver’s throwing a tantrum. Don’t fight it. Rest. Eat bland. Hydrate. And for god’s sake, write down every pill, supplement, and herbal tea you’ve ever taken - even that ‘harmless’ ginger tea your aunt swears by. I’ve seen people get wrecked because they forgot they took turmeric. Your liver doesn’t care if you think it’s ‘natural.’ It only cares if it’s toxic.
Steve and Charlie Maidment
Why do people act like this is some groundbreaking discovery? I’ve been on antivirals since 2010. This is just the same old thing with a fancy name and a higher price tag. And don’t get me started on the ‘12-week follow-up’ - like we’re all gonna remember to show up. Most people are just happy to be done with the pills and never think about it again. Then they get sick a year later and wonder why. It’s not the drug’s fault - it’s the system’s. No one holds your hand after the cure. You’re just… supposed to know what to do next. And that’s bullshit.
Michael Petesch
I’m curious - how does the prevalence of hepatitis B co-infection in the U.S. population compare to that in Southeast Asia, where HBV is endemic? Given that ledipasvir can trigger reactivation, and given that HBV is often asymptomatic for decades, is there a standardized protocol for screening across different global healthcare systems? Or is this still a patchwork of local guidelines, leaving many at risk?
Ellen Calnan
I’m 61. Diagnosed with HCV in 2022. Took Harvoni. Felt like I was slowly drowning for the first three weeks. Then one morning - I woke up and my hands didn’t shake. I walked to the mailbox without stopping. I cried. Not because I was cured - but because I remembered what it felt like to be alive. This isn’t just medicine. It’s a second chance. Don’t waste it. Write down your meds. Skip the booze. Tell your doctor about every pill, every tea, every ‘natural remedy.’ And if you’re scared? You’re not alone. We’re all in this together. You’ve got this.
Richard Risemberg
Let me tell you about my cousin - brilliant guy, 58, ex-military, never missed a workout. Took Harvoni. Felt fine until week 6 - then started seeing double. Went to the ER. Turned out he’d been taking St. John’s Wort for ‘mood support’ since his divorce. The herb tanked his ledipasvir levels. He didn’t clear the virus. Had to restart treatment. He’s now on a new regimen - and he’s sober. No more herbal nonsense. No more ‘I’m fine.’ He learned the hard way: your body doesn’t care if it’s ‘natural.’ It cares if it’s safe. So if you’re taking anything - even a vitamin - tell your doctor. No exceptions. Not even if it’s ‘just a little.’