Every year, thousands of people accidentally take too much medication-not because they meant to, but because they used a pill organizer wrong. It sounds simple: dump your pills into a little box with compartments for morning, noon, night, and Sunday through Saturday. But if you don’t follow the right steps, that box becomes a ticking time bomb. You might think you’re helping yourself stay on track, but without proper care, you could be setting yourself up for a dangerous overdose.
Why Pill Organizers Can Be Dangerous
Pill organizers aren’t magic. They’re tools. And like any tool, they can help-or hurt-depending on how you use them. The CDC says medication errors lead to over 7,000 deaths in the U.S. every year. A 2022 study in the Journal of the American Geriatrics Society found that improper use of pill organizers increases overdose risk by 23% in older adults. That’s not a small number. It means if you’re filling your organizer without checking your prescriptions, you’re more likely to make a mistake than if you didn’t use one at all. The biggest danger? Mixing up “as needed” meds with your daily ones. If you put painkillers, sleep aids, or anti-anxiety pills into the same compartments as your blood pressure or diabetes meds, you might grab the wrong one and take it twice. One Reddit user shared how they accidentally took three doses of a painkiller in one day because they didn’t realize the organizer had it labeled as a daily pill. That landed them in the ER. Another problem? Old or worn-out organizers. If the compartments are cracked, sticky, or faded, pills can stick together, labels can peel off, and you might not even know what’s inside. The National Council on Aging found that 28% of seniors are still using organizers that are over 10 years old. That’s not just outdated-it’s unsafe.What Kind of Pill Organizer Should You Use?
Not all pill boxes are the same. There are three main types:- Basic weekly (7 days, 1 time per day): $3-$9. Good for people taking one pill per day.
- Multi-dose daily (7 days, 2-4 times per day): $5-$15. Best for most people on multiple medications.
- Electronic with alarms: $25-$100. Comes with timers, lights, and sometimes even remote alerts for caregivers.
Where Not to Store Your Pill Organizer
You might think the bathroom is the most convenient spot. After all, you brush your teeth there every morning and night. But that’s exactly why it’s the worst place. Steam from showers, humidity from sinks, and temperature swings can ruin your pills. Kaiser Permanente found that storing medications in the bathroom leads to 47% faster degradation. Pills can become sticky, crumbly, or lose their strength. The same goes for storing them near the stove, in a car, or in direct sunlight. The safest place? A cool, dry drawer in your bedroom or kitchen-away from moisture and heat. Keep it below 86°F (30°C) and under 60% humidity. If you’re unsure, check the original bottle. It should say storage requirements like “store at room temperature” or “keep refrigerated.” If it says the latter, don’t put it in the organizer at all.How to Fill Your Pill Organizer Correctly
Filling your organizer isn’t a 5-minute chore. It’s a safety ritual. Follow these five steps every time:- Start with your current medication list. Don’t rely on memory. Pull out your printed list from your doctor or pharmacy. If you don’t have one, call your pharmacy and ask for an updated list. This is your bible.
- Wash your hands. Use soap and water for at least 20 seconds. You’re handling medicine-clean hands prevent contamination.
- Organize your bottles by time of day. Put all morning pills together, all afternoon pills together, etc. This keeps you from mixing up times.
- Fill one medication at a time. This is the most important step. Don’t grab all your pills and dump them in. Take one bottle, read the label, count the pills, and place them in the correct compartment. Then move to the next one. Memorial Sloan Kettering Cancer Center says this cuts double-dosing errors by 63%.
- Triple-check before closing. Look at your medication list → check the bottle label → verify the compartment. If something doesn’t match, stop. Call your pharmacist.
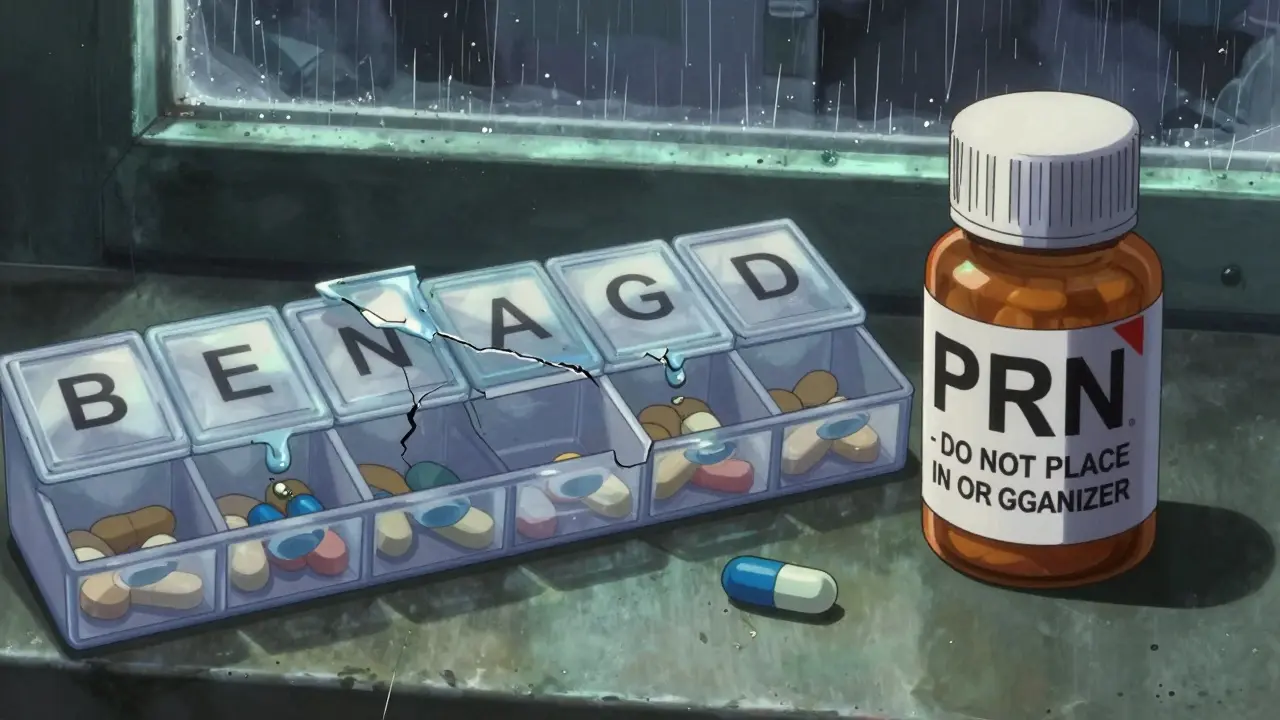
Never Put “As Needed” Pills in Your Organizer
This mistake causes 41% of all organizer-related overdoses, according to Memorial Sloan Kettering. “As needed” (PRN) medications like ibuprofen, lorazepam, oxycodone, or zolpidem should never go in your daily compartments. Why? Because you don’t take them at set times. You take them when you need them. If they’re in your morning slot, you might think, “I already took my pain pill today,” and skip it when you really need it. Or worse-you take it again because you forgot you already did. Instead, keep PRN pills in their original bottles, clearly labeled, and store them separately. Put them in a different drawer, or even a small ziplock bag with a note: “FOR USE ONLY WHEN NEEDED.” Add a sticky note on your organizer: “PRN MEDS NOT IN BOX.”Keep Original Bottles Nearby
One of the biggest mistakes people make is throwing away the original pill bottles after filling their organizer. That’s a huge risk. If you’re confused about what you took, you can’t check the label. WebMD found that 28% of errors happen because people refill their organizer using outdated labels instead of their current medication list. Always keep the original bottles within arm’s reach while you’re filling your organizer. Even after you’re done, keep them nearby-on the counter, next to your organizer, or in the same drawer. If you ever feel unsure, go back to the bottle. It has the dose, the name, the expiration date, and the pharmacy’s contact info.Watch Out for Look-Alike Pills
If you take two pills that look almost identical-say, two different blue capsules-you’re at risk. A 2025 NHCHC survey found that 63% of users struggle to tell similar pills apart. That’s why so many people grab the wrong one. Solutions?- Use a pill splitter with color-coded inserts.
- Buy separate organizers for look-alike meds-one for your blood pressure pills, another for your cholesterol pills.
- Write the name of the pill on a small piece of tape and stick it to the compartment lid.
What to Do If You Think You Overdosed
If you took too much-whether it’s one extra pill or three-you need to act fast. Don’t wait. Don’t hope it’ll pass.- Call Poison Control at 1-800-222-1222 (U.S.) or your local emergency number.
- Have your pill organizer and all medication bottles ready. They’ll ask for names, doses, and times.
- Don’t induce vomiting unless instructed.
- If you’re dizzy, confused, or having trouble breathing, call 911.
When to Ask for Help
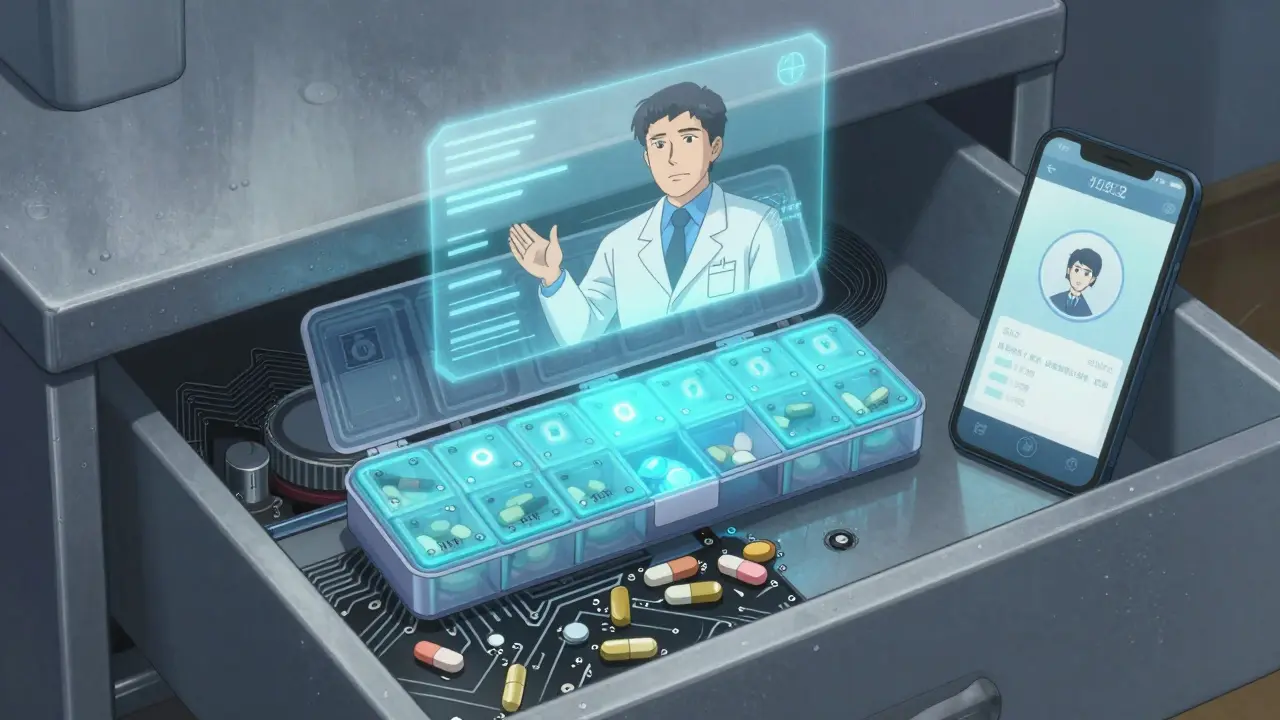
You don’t have to do this alone. Most pharmacies now offer free pill organizer filling services. A pharmacist will sit with you, check your meds against your list, and fill the box for you. That cuts errors by 52%, according to Pharmacy Times. If you’re caring for someone else-like a parent or spouse-ask the pharmacist to show you how to do it right. Many hospitals, especially cancer centers like Memorial Sloan Kettering, now require patients to have their organizers checked before discharge. And if you’re forgetful, overwhelmed, or have vision problems, consider a smart organizer with alarms, lights, or remote monitoring. Hero Health’s latest model (version 3.2.1) sends alerts to your phone if someone opens a compartment too often-like if they took two doses within four hours.Final Safety Checklist
Before you close your organizer, ask yourself:- Did I use my current medication list-not an old one?
- Did I fill one pill at a time?
- Did I leave PRN meds out of the box?
- Are all original bottles nearby?
- Is the organizer stored in a cool, dry place?
- Did I check for look-alike pills and label them?
- Did I wash my hands before handling pills?
Pill organizers are meant to keep you safe. But safety doesn’t come from the box-it comes from how you use it. Take the time. Double-check. Ask questions. Your life depends on it.
Can I put all my pills in one organizer?
No-not all pills belong in organizers. Avoid putting liquids, refrigerated meds, chewables, soft gels, or capsules that dissolve easily in them. Only use organizers for solid oral pills that don’t require special storage. Always check with your pharmacist before transferring any medication.
Is it safe to refill my pill organizer from old pill bottles?
No. Never refill your organizer using old bottle labels. Medication lists change. Doses get adjusted. New prescriptions replace old ones. Always use your most current medication list from your pharmacy or doctor. Using outdated labels is the second most common cause of pill organizer overdoses.
Should I keep my pill organizer in the bathroom?
No. Bathrooms are too humid. Steam from showers can damage pills, making them sticky, crumbly, or less effective. Store your organizer in a cool, dry place like a bedroom drawer or kitchen cabinet-away from sinks, showers, and windows.
Can I put painkillers or sleep aids in my pill organizer?
Never put “as needed” medications like ibuprofen, oxycodone, or zolpidem into your daily compartments. These should stay in their original bottles, labeled clearly, and stored separately. Putting them in the organizer causes confusion and leads to accidental overdoses.
How often should I clean my pill organizer?
Clean it every week when you refill it. Use warm water and mild soap. Dry it completely before adding new pills. If compartments are cracked, sticky, or faded, replace the organizer. Old, damaged organizers increase the risk of misidentification and contamination.
Are electronic pill organizers worth the cost?
Yes-if you forget doses, have trouble reading small labels, or live alone. Electronic organizers with alarms, lights, and remote alerts reduce missed doses by up to 44%. Medicare covers them for people with four or more chronic conditions. For many, the cost is worth the safety and peace of mind.

Kristen Russell
Just filled my organizer this morning-followed every step. Life-changing advice. Seriously, this post saved me from a disaster.
Heather Josey
I appreciate how thorough this is. As a nurse, I’ve seen too many seniors mix up PRN meds in their organizers. The part about keeping original bottles nearby? Crucial. I hand out printed checklists to my patients now-same format as your checklist. Works wonders.
Donna Peplinskie
Thank you, thank you, thank you-for writing this with such care! I’ve been helping my mom manage her meds, and she’s been using the same organizer since 2015… it’s cracked, the labels are peeling, and she swears the blue pill is her blood pressure med… but the bottle says it’s cholesterol. I cried reading your section on look-alike pills. We’re getting a new one tomorrow-with the QR codes. And I’m washing my hands before every refill. No more excuses.
Bryan Anderson
This is one of the most well-researched, practical guides I’ve seen on medication safety. The 63% reduction in double-dosing from filling one pill at a time is backed by solid data from Memorial Sloan Kettering, and it’s something most people overlook. I’ve shared this with my aging parents and my book club. The bathroom storage warning alone deserves a public service announcement. Also, kudos for mentioning Medicare coverage-many don’t know smart organizers are now eligible.
jaspreet sandhu
Everyone’s acting like this is revolutionary. Look, I’ve been taking pills for 20 years. I don’t need a 5-step ritual. I just remember what I take. You’re overcomplicating it. People get confused because they’re not paying attention, not because the organizer’s bad. Also, why are we trusting pharmacists to fill our meds? Who checks their work? It’s a system built on trust, and trust is a luxury. I take my meds when I feel like it. That’s freedom.
Alex Warden
USA has the best healthcare system in the world, but we still need a guide to not overdose on pills? What’s next, a manual for not eating expired food? This is why America’s falling apart-people can’t even read labels. In my country, we just take the pills and trust the doctor. No boxes. No alarms. No handwashing. Just discipline. You people need to toughen up.
LIZETH DE PACHECO
I used to be the person who threw away the bottles. Then I took two doses of my anxiety med because I forgot I already took it. I spent 4 hours in the ER. This post? It’s the reason I’m alive today. I keep my bottles next to my organizer, I label everything, and I refill every Sunday like clockwork. If you’re reading this and you’re scared to do it right-just start with one step. Wash your hands. Then do the next. You’ve got this.
Lee M
It’s not the organizer that’s dangerous-it’s the system. Why do we even need these things? Why isn’t the pharmacy just giving us one pill a day in a blister pack? Why are we forced to manage our own meds like a puzzle? This is capitalism’s answer to elder care: give them a box and tell them to figure it out. We’re treating human beings like machines. And then we act shocked when they break.
Matthew Hekmatniaz
As someone who moved from Iran to the U.S. and had to navigate this system, I can say this: the clarity here is rare. In my home country, we rely on family to manage meds. Here, it’s all on you. This guide bridges that gap. I showed it to my neighbor, who’s blind-she’s getting a voice-enabled organizer next week. The QR code idea? Brilliant. Simple, human, and scalable. Thank you for writing this like you care.
Olukayode Oguntulu
Ah, the modern pathology of pharmaceutical compliance: a ritualized, bureaucratic dance with mortality. We are not merely taking pills-we are enacting a neoliberal sacrament of self-surveillance. The pill organizer becomes the altar, the pharmacist the priest, and the CDC the oracle. We sanitize our hands, label our compartments, and yet-still, we are alienated from the very substances meant to sustain us. The real overdose? The illusion of control. The box does not save you. It merely delays the inevitable entropy of the body. But, of course, you must still wash your hands. For propriety’s sake.
Liam George
Did you know the FDA allows pill organizers to be sold without tamper-proof seals? That’s because they’re in cahoots with Big Pharma. The real reason they want you to use these boxes? So they can track your compliance. Your smart organizer? It’s sending data to your insurer. They’ll raise your premiums if you miss a dose. And those QR codes? They’re not for pill identification-they’re for biometric logging. I’ve seen the documents. They’re using this to build a pharmacological surveillance state. Don’t trust the organizer. Don’t trust the pharmacist. Burn the box. Take your meds from the bottle. And pray.