HIV Medication & Birth Control Interaction Checker
Check Your Birth Control Options
Select your HIV medications to see which birth control methods are safe and effective.
Select your HIV medications and click "Check My Options" to see results.
For women living with HIV, HIV protease inhibitors are a critical part of treatment, but they can interfere with birth control effectiveness. This interaction isn't just theoretical-it's a documented risk that has led to unintended pregnancies.
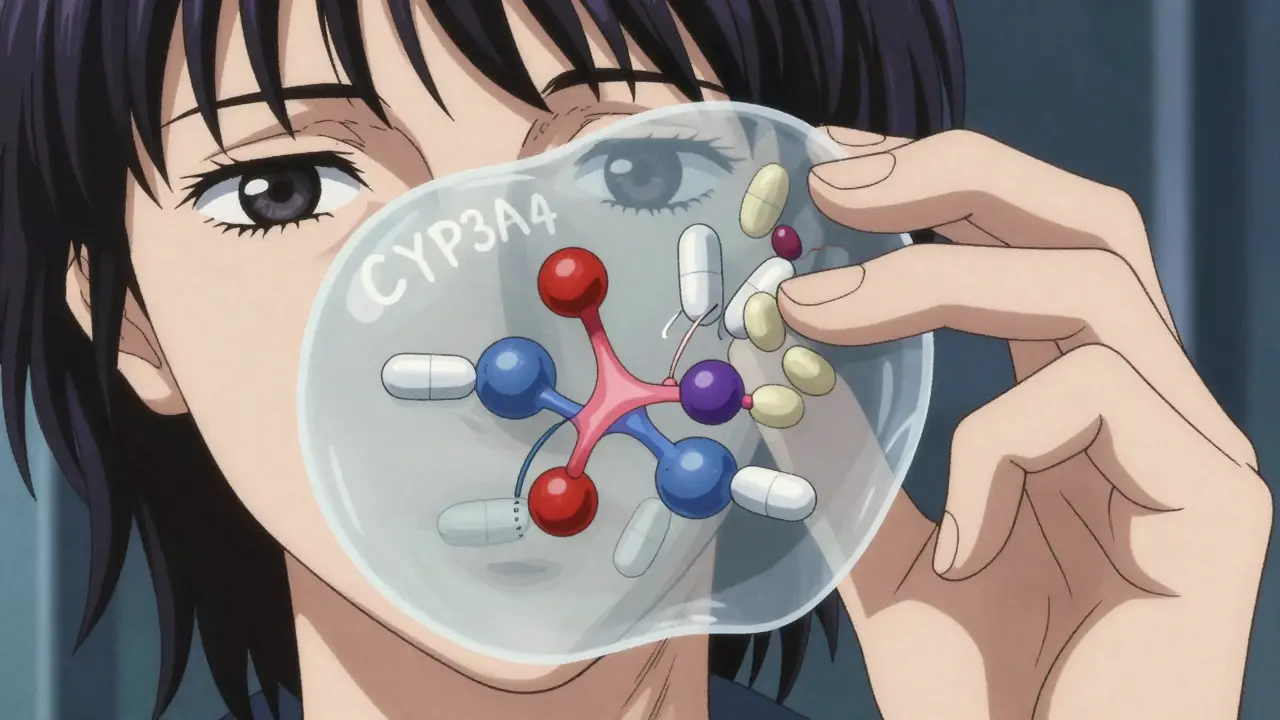
How HIV Protease Inhibitors Interfere with Birth Control
HIV protease inhibitors work by blocking enzymes that HIV needs to replicate. However, they also affect the same enzymes used by your body to process contraceptive hormones. Specifically, they interact with the CYP3A4 enzyme system, which metabolizes hormones like estrogen and progestin. This disruption can cause contraceptive hormone levels to drop too low, making birth control less effective. For example, when using a ritonavir-boosted protease inhibitor like lopinavir/ritonavir, studies show ethinyl estradiol levels (a key hormone in many birth control pills) can drop by 45% or more. This means your body might not get enough hormones to prevent ovulation or thicken cervical mucus, increasing pregnancy risk.
Specific Drug Interactions and Their Effects
Different HIV medications interact with birth control in unique ways. A 2010 AIDS Clinical Trial Group study (A5188) found that women using the contraceptive patch with lopinavir/ritonavir experienced a 45% decrease in ethinyl estradiol and an 83% increase in norelgestromin. Meanwhile, a 2019 Lancet study revealed that efavirenz-containing regimens caused 79% lower etonogestrel and 59% lower ethinyl estradiol levels compared to controls. The contraceptive ring (NuvaRing) is particularly vulnerable: 38% of women using efavirenz-based regimens had subtherapeutic etonogestrel levels, meaning the ring wasn't working properly.
| Contraceptive Method | With Ritonavir-Boosted PIs | With Dolutegravir |
|---|---|---|
| Combined Oral Contraceptive (COC) | 45-83% reduction in hormone levels | No significant change |
| Contraceptive Patch | 45% lower ethinyl estradiol | Minimal effect |
| Contraceptive Ring (NuvaRing) | 38% of women at subtherapeutic levels | Minimal effect |
| Intrauterine Device (IUD) | 99% effective | 99% effective |
| Implant (Nexplanon) | 40-60% reduction in hormone levels | Safe and effective |
What Health Organizations Say About This Risk
The World Health Organization (WHO) and U.S. Centers for Disease Control and Prevention (CDC) have clear guidelines based on solid evidence. According to WHO's 2015 Medical Eligibility Criteria for Contraceptive Use, progestin-only pills combined with ritonavir-boosted protease inhibitors fall under Category 3-meaning the risks usually outweigh the benefits. The CDC's 2017 systematic review of 32 studies reinforced this, noting that hormonal contraceptives are unreliable with certain HIV drugs. Both organizations strongly recommend non-hormonal options like copper IUDs or implants for women on protease inhibitors. They also emphasize that these interactions are well-documented and should be part of routine counseling for HIV-positive individuals.
Safe Contraceptive Options for Women on HIV Medications
Not all birth control methods are affected by HIV medications. Intrauterine devices (IUDs), both hormonal and copper, maintain 99% effectiveness regardless of the antiretroviral regimen. Implants like Nexplanon work well with dolutegravir-based treatments but may have reduced effectiveness with ritonavir-boosted regimens. Non-hormonal methods like condoms or diaphragms are reliable alternatives. A 2022 Guttmacher Institute report found that 68% of HIV-positive women in high-income countries use long-acting reversible contraceptives (LARCs), but this drops to 22% in low-income regions due to access barriers. If you're on HIV treatment, always discuss your contraceptive options with your provider-they can help you choose a method that won't interfere with your medication.
Real-World Consequences and Case Examples
This isn't just a lab finding-it happens in real life. On the HIV.gov forum, a user named MariaJ reported becoming pregnant while using Tri-Sprintec (a combined oral contraceptive) with darunavir/cobicistat, despite perfect adherence to both medications. The Positive Women's Network-USA 2021 survey of 327 HIV-positive women found that 28% experienced contraceptive failure while using hormonal methods with antiretrovirals, with 63% of those cases involving protease inhibitors. One Reddit user described using Depo-Provera with atazanavir/ritonavir and becoming pregnant at 18 weeks gestation, with their provider confirming the interaction was "well-documented but often overlooked in community clinics." These stories highlight the urgent need for better education and counseling around this issue.

What Healthcare Providers Need to Know
Clinicians must actively address contraceptive interactions during HIV care. The Reproductive Health Access Project recommends spending 7-10 minutes specifically discussing these risks during family planning consultations. Providers should use tools like the CDC's 2022 interaction checker, which covers 147 drug pairs. ACOG's teach-back method-where patients explain their understanding in their own words-has proven effective: 85% of patients correctly described alternative options after this technique versus 42% with standard counseling. Training matters too: the CDC's 2-hour online course "Contraceptive Considerations for HIV-Positive Women" has trained over 8,000 providers globally, with post-test scores showing 92% mastery of critical interaction knowledge. These steps ensure patients receive accurate, actionable advice.
Future Developments and Improvements
The field is evolving. The WHO's 2023 draft guidelines suggest reclassifying etonogestrel implants as safe for use with dolutegravir-based regimens, based on new data showing only 12% hormone reduction. The NIH-funded NEXT-Study (NCT04578291) is currently testing levonorgestrel IUDs with 12 different antiretroviral regimens across 15 countries. By 2030, the Global Health Council predicts 95% of contraceptive counseling for HIV-positive women will occur through integrated "one-stop-shop" clinics, up from 47% in 2022. This shift could reduce contraceptive failure rates from 9.3 to 3.1 per 100 woman-years. However, challenges remain: a 2024 report noted 35% lower levonorgestrel concentrations with darunavir/cobicistat, which may compromise emergency contraception efficacy. As dolutegravir becomes the first-line treatment for 72% of new HIV cases, these interactions are becoming less common-but awareness is still crucial.
Can I use birth control pills while taking HIV protease inhibitors?
No, most hormonal birth control pills are not safe with HIV protease inhibitors. Ritonavir-boosted regimens like lopinavir/ritonavir can reduce hormone levels by up to 83%, making them unreliable. The WHO classifies this combination as Category 3, meaning it's not recommended unless no other options exist. Instead, consider non-hormonal methods like copper IUDs or implants that work safely with these medications.
What are the safest birth control options for women with HIV?
Intrauterine devices (IUDs), both hormonal and copper, are the safest options. They maintain 99% effectiveness regardless of the HIV medication regimen. Implants like Nexplanon also work well with dolutegravir-based treatments but may have reduced effectiveness with ritonavir-boosted regimens. Non-hormonal methods like condoms or diaphragms are reliable alternatives. Always discuss your options with a healthcare provider who understands these interactions.
How do I know if my birth control is affected by my HIV medications?
Check the specific HIV medications you're taking. Ritonavir-boosted protease inhibitors (like lopinavir/ritonavir) and efavirenz are high-risk for interactions with hormonal contraceptives. Integrase inhibitors like dolutegravir typically have minimal effects. Use the CDC's interaction checker tool or ask your provider to review your regimen. If you're unsure, switch to non-hormonal methods like IUDs or condoms to be safe.
What should I do if I'm already on HIV meds and birth control?
Contact your healthcare provider immediately. They can assess your specific medications and recommend safer alternatives. Do not stop taking your HIV treatment without guidance, as this risks viral rebound. If you're using hormonal birth control with a high-risk HIV medication, switch to a non-hormonal method like an IUD or condoms. Your provider can help you transition safely without interrupting your HIV care.
Are there any new developments in this area?
Yes! The WHO's 2023 draft guidelines suggest reclassifying etonogestrel implants as safe for use with dolutegravir-based regimens, based on new data showing only 12% hormone reduction. The NIH-funded NEXT-Study is currently testing levonorgestrel IUDs with 12 different antiretroviral regimens across 15 countries. By 2030, integrated clinics could reduce contraceptive failure rates from 9.3 to 3.1 per 100 woman-years. However, darunavir/cobicistat still poses risks, with a 2024 report showing 35% lower levonorgestrel levels that may compromise emergency contraception.