Penicillin Allergy Risk Calculator
Is Your Penicillin Allergy Label Accurate?
This tool helps determine your risk of having a true penicillin allergy based on your reaction history. Over 95% of people labeled allergic to penicillin are actually not allergic.
Your risk assessment results will appear here.
More than 10% of people in the U.S. say they’re allergic to penicillin. But here’s the truth: 95% of them aren’t. That’s not a typo. Most of these labels stuck from a childhood rash, a stomach upset, or a doctor’s guess - not a real allergy. And because of it, people are getting worse antibiotics, spending more money, and facing higher risks of deadly infections like C. difficile.
When someone says they’re allergic to penicillin, doctors often avoid all beta-lactam antibiotics - including cephalosporins like ceftriaxone. But the fear of cross-reactivity is outdated. Modern science shows the real risk is tiny: just 1% to 3% for first-gen cephalosporins, and even less for newer ones. So why are so many patients still being denied safe, effective drugs? The answer lies in outdated assumptions, poor documentation, and a lack of testing.
What Exactly Is a Beta-Lactam Allergy?
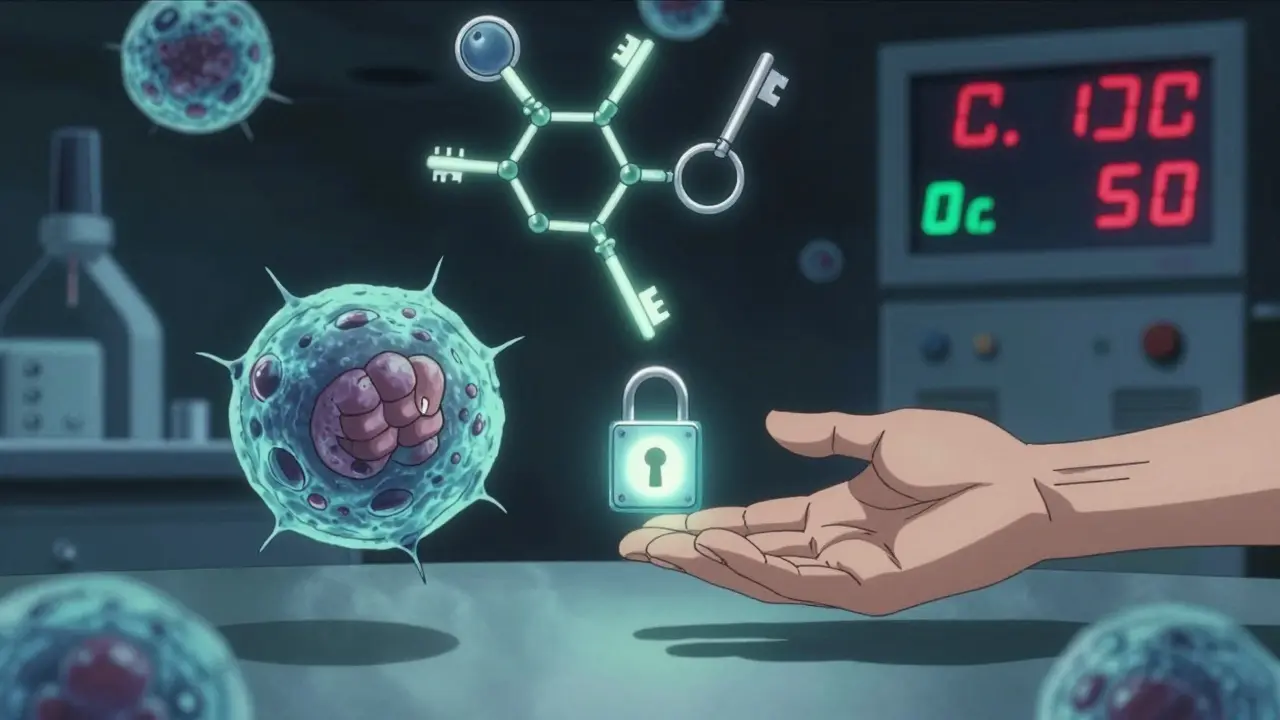
Beta-lactam antibiotics share a core chemical structure - a four-membered ring called the beta-lactam ring. This includes penicillins (like amoxicillin and ampicillin), cephalosporins (like cefalexin and ceftriaxone), and a few others. The allergy isn’t to the whole class - it’s to how your immune system reacts to specific parts of the molecule.
True IgE-mediated allergies happen within minutes to an hour after taking the drug. Symptoms? Hives (in 90% of cases), swelling of the face or throat (angioedema in 50%), trouble breathing (30%), and in rare cases, full-blown anaphylaxis (0.01% to 0.05% of courses). These are life-threatening. But most people who say they’re allergic never had any of these. They had a rash from a virus, nausea from an empty stomach, or a headache that had nothing to do with the antibiotic.
Here’s the kicker: if you were labeled allergic 20 years ago, there’s an 80% chance you’ve lost that allergy by now. Your immune system forgets. But your chart doesn’t.
Penicillin Allergy: The Most Misunderstood Label
Penicillin is the most common drug allergy reported - but also the most overdiagnosed. The American Academy of Allergy, Asthma & Immunology says 10% of people claim a penicillin allergy. Yet when tested properly, only 1% to 2% actually have a true IgE-mediated reaction.
How do you know if it’s real? Two tests: skin prick and intradermal testing. Done together, they’re 97% to 99% accurate at ruling out a true allergy. If both are negative, you can safely take penicillin again. No need for guesswork.
And if testing isn’t available? A graded oral challenge works just as well. Give 10% of the dose, wait 30 minutes. Then 30%, then 60%. Watch for symptoms. If none appear, you’re not allergic. This is what Yale Medicine and Mayo Clinic do routinely. In fact, Mayo’s system-wide program in 2022 successfully delabeled 65% of patients who had been told they were allergic for decades.
And here’s the cost: if you’re wrongly labeled, you’re 70% more likely to get a broader-spectrum antibiotic like vancomycin or clindamycin. These drugs are more expensive, harder on your gut, and linked to higher rates of C. difficile - a dangerous infection that causes severe diarrhea and can kill. The CDC says this mislabeling adds $2,000 to $4,000 in extra costs per patient every year.
Cephalosporins: The Overlooked Safe Option
Many doctors still avoid cephalosporins in patients with penicillin allergies. But that’s based on old data. In the 1980s, people thought cross-reactivity was 10% to 30%. Today? It’s 1% to 3% for first-generation cephalosporins like cefazolin. For later generations - like ceftriaxone, cefdinir, or cefixime - the risk is nearly zero.
Why? Because later cephalosporins have different side chains. The part of the molecule that triggers the immune response? It’s not the same as penicillin’s. Think of it like this: penicillin and cephalosporin are like two different keys. They both open the same lock (the beta-lactam ring), but only one key fits your lock (your immune system). The other? It’s useless.
There’s no standard skin test for cephalosporins because commercial reagents don’t exist. But that doesn’t mean you can’t take them. If you have a low-risk history - like a rash from childhood, no breathing issues, no anaphylaxis - you can often take a cephalosporin safely. Many hospitals now use direct oral challenges for these cases.
And here’s the reality: in emergency situations - like a serious infection after surgery - you need a cephalosporin. Avoiding it because of an unverified penicillin label puts you at greater risk than taking it.

What Happens If You Really Are Allergic?
Some people have real, life-threatening reactions. For them, penicillin is off-limits. But even then, there’s a solution: desensitization.
Desensitization isn’t a cure. It’s a temporary override. You’re given tiny, increasing doses of penicillin over 4 to 8 hours - under strict medical supervision. Your immune system gets tricked into ignoring the drug. It works in over 80% of cases. This is how pregnant women with syphilis get penicillin - the only drug that cures it. It’s how someone with neurosyphilis gets treated. And it’s how patients with severe infections get the best possible antibiotic.
But this isn’t something you do at your local clinic. It requires an allergist, IV access, epinephrine on standby, and a monitored inpatient setting. The CDC is clear: “Desensitization protocols to penicillin should be performed by allergists.”
For cephalosporins, desensitization is possible too - but less studied. It’s used when there’s no alternative, like in severe MRSA infections where cefazolin is the only effective option.
How to Get Your Label Removed
If you were told you’re allergic to penicillin as a kid - especially if it was just a rash - you should get tested. Here’s how:
- Find an allergist or an antimicrobial stewardship program. Many hospitals now have them.
- Bring your full history: What happened? When? Did you have hives? Swelling? Trouble breathing? Or just a rash? Was it after a viral illness?
- Ask for skin testing. If it’s negative, you’ll likely get an oral challenge with amoxicillin.
- If you pass, your chart gets updated. No more “penicillin allergy.”
Some clinics even do this without skin testing if your history is low-risk. A 2023 study from Brigham and Women’s Hospital showed that giving a full dose of amoxicillin to patients with only a past rash - no other symptoms - was safe in over 95% of cases.
And the benefits? They’re huge. Patients who get delabeled:
- Get better antibiotics
- Have fewer hospital readmissions
- Lower their risk of C. difficile by up to 17%
- Save thousands in avoidable costs
The Bigger Picture: Why This Matters
This isn’t just about one drug. It’s about antibiotic resistance. When we avoid penicillin and cephalosporins unnecessarily, we turn to drugs like vancomycin, fluoroquinolones, or carbapenems. These are last-resort antibiotics. Overuse leads to superbugs. We’re already seeing more cases of drug-resistant infections.
Hospitals with formal allergy delabeling programs cut broad-spectrum antibiotic use by 23%. C. difficile infections dropped 17%. That’s not just better care - that’s saving lives.
And the future is getting clearer. Researchers are testing blood markers like IL-4 and IL-13 to predict penicillin allergies without skin tests. A $12.5 million NIH study is launching in 2026 to test streamlined allergy evaluations in community clinics. This could bring testing to rural areas where allergists are scarce.
Right now, only 35% of U.S. hospitals have formal allergy assessment programs. Only 28% of rural hospitals have access to allergists. But awareness is growing. The CDC, the American Academy of Allergy, and the Infectious Diseases Society of America all agree: fixing penicillin mislabeling is one of the biggest wins we have in antibiotic stewardship.
What You Should Do Now
If you’ve been told you’re allergic to penicillin:
- Check your records. Was it a rash? Did you have trouble breathing? Was it more than 10 years ago?
- Ask your doctor: “Could this be mislabeled?”
- Request a referral to an allergist or antimicrobial stewardship program.
- Don’t assume you’re allergic forever. Your immune system changes.
If you’re a healthcare provider:
- Stop writing “penicillin allergy” without details. Write: “Rash at age 6, no anaphylaxis, 20 years ago.”
- Offer oral challenges for low-risk patients.
- Connect with your hospital’s stewardship team. They can help.
Because here’s the bottom line: a penicillin allergy label isn’t a diagnosis. It’s a guess. And too many guesses are costing lives - and money - every single day.

Autumn Frankart
So let me get this straight - the government and Big Pharma are quietly erasing penicillin allergies from medical records so they can push cheaper antibiotics? 😏
And you’re telling me we’re supposed to trust this? No skin test? No lab validation? Just some doctor shrugging and saying, “You’re fine now”?
What about the people who actually died? What about the ones who went into anaphylaxis and were ignored because the chart said “rash at age 6”?
This isn’t science - it’s corporate triage. They don’t care if you live or die. They care if you stop using vancomycin and start using amoxicillin - which is 1/10th the price.
And don’t even get me started on how fast the CDC changed their stance right after the 2022 drug pricing bill passed.
They’re not fixing a problem - they’re covering one up. And you’re all just swallowing it because it sounds convenient.
Wake up. This is how they control the population. One “misdiagnosis” at a time.
Stephon Devereux
Look - I’ve been in emergency medicine for 22 years. I’ve seen patients die because we gave them clindamycin instead of cefazolin because of a 30-year-old rash.
Here’s the truth: allergies fade. The immune system doesn’t keep grudges. It forgets. And if you’re not testing people, you’re not practicing medicine - you’re practicing fear.
I had a patient last year - 72, told she was allergic since childhood. Skin test negative. Oral challenge - no reaction. She got ceftriaxone for her sepsis. Walked out in 48 hours. Saved $3,800. Avoided C. diff.
This isn’t theory. It’s daily practice in hospitals that care.
Stop letting outdated labels dictate care. Ask for testing. Push for change. Your life might depend on it.
Neha Motiwala
Wait… wait… wait… so you’re saying the whole medical system is built on a lie? That millions of people are being poisoned with dangerous drugs because someone wrote “penicillin allergy” on a chart in 1987?
And now they want us to just… take a pill? Without tests? Without consent? Without paperwork?
This is not medicine - this is eugenics by prescription.
Who benefits? Who owns the labs? Who profits when we stop using vancomycin?
There’s a reason they won’t let you see the full data. There’s a reason they don’t want you to know about the 2021 FDA memo on “low-risk delabeling.”
They’re erasing your history. And you’re letting them.
athmaja biju
As someone from India, I’ve seen this firsthand. In rural clinics, doctors still avoid cephalosporins for penicillin-labeled patients - even when it’s the only effective option.
But here’s the twist: in urban hospitals, we’ve been doing oral challenges for years - no skin test, no allergist. Just a nurse, a pill, and a 30-minute wait.
Success rate? Over 90%.
And guess what? No deaths. No lawsuits. No drama.
So why is the U.S. still stuck in 1990? Is it bureaucracy? Fear? Or just laziness?
Stop overcomplicating what’s simple: if you didn’t have anaphylaxis, you’re probably not allergic. Test it. Move on.
alex clo
The data presented here is robust, peer-reviewed, and aligns with guidelines from the AAAAI, CDC, and IDSA.
Multiple cohort studies (e.g., Brigham and Women’s 2023, Mayo Clinic 2022) demonstrate that low-risk patients can safely undergo oral challenges without prior skin testing.
Furthermore, the economic and clinical burden of unnecessary broad-spectrum antibiotic use is well-documented in the literature, with clear correlations to C. difficile incidence and antimicrobial resistance.
Recommendations for delabeling are not speculative - they are standard of care in accredited institutions.
It is incumbent upon clinicians and patients alike to prioritize evidence over anecdote, and systemic change over inherited assumptions.
Alyssa Williams
this is wild honestly i had a rash when i was 5 and they just labeled me allergic forever and now im 34 and i literally cant take any antibiotic without getting scammed into vancomycin and it costs me a fortune and makes me sicker lmao
Ernie Simsek
💀 BRO THIS IS THE MOST IMPORTANT THREAD I’VE SEEN ALL YEAR
MY MOM GOT C. DIFFICILE BECAUSE THEY GAVE HER CLINDAMYCIN INSTEAD OF AMOXICILLIN BECAUSE OF A RASH FROM 1998
SHE WAS IN THE HOSPITAL FOR 3 WEEKS
THEY NEVER EVEN TESTED HER
AND NOW SHE’S GOT A ‘ALLERGY’ ON HER RECORD THAT’S NOT EVEN REAL
WHY ISN’T THIS ON THE FRONT PAGE OF THE NEW YORK TIMES??
WE NEED A MOVEMENT.
#DELABELTHELABEL
Joanne Tan
i just got my label removed last month!! took 3 hours, drank amoxicillin in front of a nurse, no reaction. now i can take ceftriaxone for my sinus infection. saved $2k. felt like a superhero. if you think you’re allergic and it was a childhood rash - go get tested. it’s life-changing.