What Are Anxiety Disorders?
Anxiety disorders aren’t just feeling stressed or nervous. They’re real medical conditions where fear or worry becomes so intense and constant that it stops you from living your life. You might feel your heart racing for no reason, avoid social events because you’re terrified of being judged, or spend hours checking if you locked the door-even when you know you did. The anxiety disorders category includes several distinct conditions, all sharing one thing: fear that’s out of proportion to the actual danger.
According to the American Psychiatric Association’s DSM-5, these aren’t temporary nerves. They’re persistent, lasting at least six months in most cases, and interfere with work, relationships, or daily routines. About 1 in 5 U.S. adults deal with one of these disorders each year, and women are nearly twice as likely to be affected as men. It’s not weakness. It’s biology. Brain chemistry, genetics, and life experiences all play a role.
The Seven Main Types of Anxiety Disorders
Not all anxiety looks the same. Each type has its own pattern of thoughts, feelings, and behaviors.
- Generalized Anxiety Disorder (GAD): This is constant, excessive worry about everyday things-work, health, bills, even minor decisions. People with GAD often say they can’t turn off their thoughts. It’s not just being a perfectionist; it’s waking up already anxious and staying that way all day, six months or longer.
- Panic Disorder: This involves sudden, intense episodes of fear that feel like a heart attack. You might feel like you’re dying, can’t breathe, or are losing control. These panic attacks come without warning and are followed by weeks of dreading the next one.
- Social Anxiety Disorder: It’s more than shyness. This is a paralyzing fear of being watched, judged, or humiliated in social settings-even something as simple as ordering coffee or speaking up in a meeting. Many people with this condition avoid parties, public speaking, or even eating in front of others.
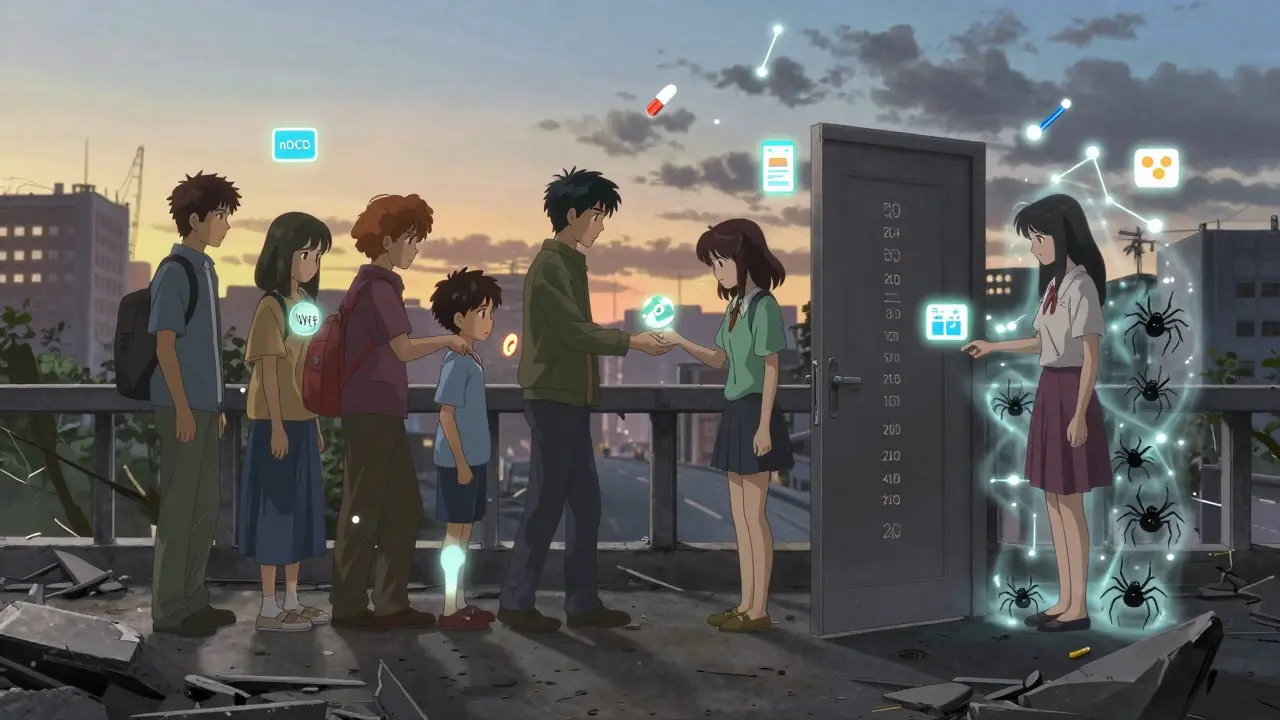
- Specific Phobias: These are extreme fears of specific things-spiders, heights, flying, needles. The fear isn’t just discomfort; it’s so strong that people will go out of their way to avoid the trigger, even if it disrupts their life.
- Obsessive-Compulsive Disorder (OCD): While now classified separately in DSM-5, OCD still fits under the anxiety umbrella. It’s not just liking things neat. It’s being trapped by unwanted, intrusive thoughts (obsessions) and feeling compelled to do rituals (compulsions) to reduce the dread-like washing hands until they bleed or checking locks 20 times.
- Separation Anxiety Disorder: Often thought of as a childhood issue, this affects adults too. It’s an overwhelming fear of being separated from loved ones, even when they’re safe. People may refuse to travel, stay home constantly, or panic when their partner leaves the room.
- Selective Mutism: This mostly affects children. They speak normally at home but stay completely silent in school or social settings-even when they want to speak. It’s not defiance; it’s extreme anxiety locking their voice.
Common Symptoms Across All Types
Even though the triggers differ, the body reacts in similar ways. Physical symptoms are often the first thing people notice-and they’re real.
- Heart rate spikes to 110-140 beats per minute during panic attacks
- Sweating (reported by 92% of panic disorder patients)
- Trembling or shaking (87%)
- Shortness of breath (83%)
- Dizziness or lightheadedness (76%)
- Nausea or stomach upset (68%)
Cognitive symptoms are just as disabling:
- Racing thoughts (82%)
- Difficulty concentrating (89% in GAD)
- Catastrophic thinking-imagining the worst possible outcome
- Rumination-replaying the same worry over and over
Emotionally, people often feel like they’re on the edge of collapse. A sense of impending doom hits during panic attacks (95% of cases). Fear of losing control or going crazy is common. Many describe it as being trapped in their own mind.
What Treatments Actually Work?
There’s good news: anxiety disorders respond well to science-backed treatments. The two most effective are cognitive behavioral therapy (CBT) and medication, especially SSRIs.
Cognitive Behavioral Therapy (CBT) is the gold standard. It teaches you to spot distorted thoughts and replace them with realistic ones. For example, instead of thinking, “Everyone thinks I’m awkward,” you learn to ask, “What’s the evidence for that?” CBT also includes exposure therapy-gradually facing feared situations in a controlled way. For social anxiety, that might mean starting with saying hello to a neighbor, then speaking up in a small group, then giving a short presentation. Studies show 50-60% of people see major improvement after 12-20 sessions. The best part? The skills last long after therapy ends.
SSRIs like sertraline (Zoloft) and fluoxetine (Prozac) are the first-line medications. They don’t work overnight-it takes 6-12 weeks to feel the full effect. But once they do, they reduce physical symptoms like heart palpitations and trembling. About 40-60% of people respond well. They’re safer than older drugs and don’t cause dependence.
Benzodiazepines like Xanax or Valium offer quick relief, but they’re not a long-term solution. They can be addictive, cause memory problems, and lose effectiveness over time. Doctors now reserve them for short-term use during crisis periods.
What About Newer Treatments?
The field is evolving fast. In 2023, the FDA approved zuranolone (Zurzuvae), the first oral pill specifically for postpartum anxiety, with a 54% remission rate in trials. Another promising area is Acceptance and Commitment Therapy (ACT), which helps people accept uncomfortable feelings instead of fighting them, and focus on values-driven actions. Studies show it works just as well as CBT for many.
For treatment-resistant cases, ketamine-assisted therapy is showing rapid results-in some trials, 65% of patients saw reduced anxiety within hours. It’s still experimental and not widely available, but it’s a breakthrough for those who haven’t responded to anything else.
Digital tools are also changing the game. Apps like nOCD and Wysa offer guided CBT exercises and have been shown to reduce symptoms by 35-45% in just 8 weeks. Some are even covered by Medicare now. AI tools are being tested to predict panic attacks 24 hours in advance with 87% accuracy, using voice patterns and movement data from wearables.
Why Do So Many People Struggle to Get Help?
Even with effective treatments available, most people don’t get the care they need. A 2022 VA survey found only 37% of patients reached remission after six months. Why?
- Wait times: Finding a therapist who specializes in anxiety can take 6-8 weeks.
- Cost and insurance: Many plans limit therapy sessions or don’t cover newer treatments.
- Side effects: Some people quit SSRIs because they feel emotionally flat or gain weight.
- Exposure is hard: CBT requires facing fears-and that’s scary. One Reddit user wrote, “I wanted to quit after the first exposure exercise. My heart was pounding so hard I thought I’d pass out.” But they kept going, and panic attacks dropped from 5-7 a week to 1-2.
Combined treatment-therapy plus medication-works best. A 2023 NAMI survey found 58% of people improved with both, compared to 42% with meds alone and 38% with therapy alone.
What Can You Do Right Now?
You don’t need to wait for a therapist to start feeling better. Here’s what helps immediately:
- Diaphragmatic breathing: Breathe in slowly through your nose for 5 seconds, hold for 2, then out through your mouth for 6. Do this for 2 minutes. It calms your nervous system faster than any pill.
- Grounding techniques: Use the 5-4-3-2-1 method. Name 5 things you see, 4 you can touch, 3 you hear, 2 you smell, 1 you taste. This pulls you out of your thoughts and into your body.
- Move your body: Even a 10-minute walk reduces cortisol, the stress hormone. You don’t need to run a marathon-just get moving.
- Limit caffeine and alcohol: Both worsen anxiety. Caffeine spikes heart rate; alcohol disrupts sleep and triggers rebound anxiety.
Support groups matter too. The Anxiety and Depression Association of America runs over 300 weekly groups. NAMI’s 24/7 helpline answers 25,000 calls a month. You’re not alone.
What’s the Long-Term Outlook?
Anxiety disorders are chronic, but they’re not life sentences. With the right tools, most people learn to manage symptoms and live full lives. The stigma is fading-67% of Americans now see anxiety as a medical condition, not a personal failing. That’s up from 42% in 2010.
Research is heading toward precision medicine. Scientists are identifying brain patterns that predict who will respond to CBT versus medication. Within five years, genetic tests could guide treatment choices, cutting down trial-and-error prescribing by half.
The bottom line: anxiety is treatable. It takes time, effort, and sometimes help from others-but recovery isn’t just possible. It’s proven.
Can anxiety disorders go away on their own?
Sometimes symptoms lessen over time, but they rarely disappear completely without treatment. Left untreated, anxiety often worsens or leads to other problems like depression, substance use, or avoidance behaviors that limit your life. Early intervention gives you the best chance for lasting recovery.
Is CBT better than medication for anxiety?
Both work well, but CBT has longer-lasting results. Medication helps manage symptoms while you’re taking it, but CBT teaches skills you use for life. Many people benefit most from combining both-medication to reduce the intensity of symptoms, and CBT to change the thinking patterns behind them.
Do SSRIs make you feel numb or emotionless?
Some people report emotional blunting, especially early on. It’s not universal, and it often improves after a few weeks. If it persists, talk to your doctor. Switching to a different SSRI or adding buspirone (a non-addictive anti-anxiety medication) can help. Never stop SSRIs suddenly-always taper under medical supervision.
How long does CBT take to work?
Most people start noticing changes after 4-6 weeks, with major improvement by session 12. CBT typically lasts 12-20 weekly sessions. The key is consistency-doing the homework between sessions. Skipping practice slows progress.
Can kids and teens have anxiety disorders too?
Yes. Half of all anxiety disorders begin by age 11. In children, it might look like school refusal, tantrums, or physical complaints like stomachaches with no medical cause. Early treatment is critical-it prevents long-term struggles and helps them build coping skills before bad habits take root.
Are anxiety disorders genetic?
Genetics play a role-if a close relative has an anxiety disorder, your risk is higher. But environment matters too. Trauma, chronic stress, or growing up in a highly critical household can trigger it, even without a family history. It’s a mix of nature and nurture.
Can digital apps replace therapy?
Apps like nOCD or Wysa are excellent supplements-they offer CBT exercises, tracking, and support when you can’t see a therapist. But they’re not a full replacement for personalized care, especially for severe cases. Use them as a bridge or reinforcement, not the only treatment.
Next Steps: What to Do If You or Someone You Know Is Struggling
If you recognize these symptoms in yourself or someone else, don’t wait. Start with your doctor. Ask for a referral to a psychologist or psychiatrist who specializes in anxiety. Look for someone trained in CBT or ACT. If cost is a barrier, check community clinics, university training centers, or online therapy platforms with sliding-scale fees.
Track your symptoms for a week-note when panic hits, what you were doing, how you reacted. This helps your therapist understand your patterns. And remember: asking for help isn’t giving up. It’s the bravest thing you can do.
