Every time you take an antibiotic when you don’t need it, you’re not just helping yourself-you’re helping bacteria get stronger. That’s the quiet, dangerous truth behind antibiotic overuse. It’s not just about one bad pill. It’s about millions of pills, prescribed too easily, taken too often, and used in ways that let dangerous bacteria evolve into untouchable threats.
What Happens When Antibiotics Don’t Work Anymore
Antibiotics are powerful tools-but only when they’re used right. When they’re overused, bacteria learn to survive them. This isn’t science fiction. It’s happening right now. According to the World Health Organization, one in six confirmed bacterial infections worldwide in 2023 were resistant to standard antibiotics. That number has been rising by 5% to 15% every year since 2018. In some regions, like South Asia and the Eastern Mediterranean, it’s worse: one in three infections no longer respond to first-line drugs. Take Escherichia coli, a common cause of urinary tract infections. In many places, 42% of these infections are now resistant to third-generation cephalosporins, one of the most common treatments. For Staphylococcus aureus, nearly one in three cases are now methicillin-resistant (MRSA), meaning common antibiotics like penicillin and amoxicillin won’t touch them. And it’s not just old drugs failing-last-resort antibiotics like carbapenems are losing their power too. Experts predict resistance to these final options will double by 2035 compared to 2005 levels. This isn’t just a hospital problem. It’s everywhere. A simple cut can turn deadly. A routine surgery becomes risky. Chemotherapy patients, who rely on antibiotics to fight off infections while their immune systems are down, are now facing higher chances of untreatable infections.C. difficile: The Silent Killer Behind the Antibiotic Curtain
When you take an antibiotic, it doesn’t just kill the bad bacteria. It wipes out the good ones too-especially in your gut. That’s when Clostridioides difficile, or C. difficile, moves in. It’s not a new bacteria. It’s always been there, quietly waiting. But antibiotics give it the opening it needs. C. difficile causes severe diarrhea, fever, and abdominal pain. In serious cases, it leads to colon damage, sepsis, and death. In 2017, the CDC reported nearly half a million C. difficile infections in the U.S. alone, with around 29,000 deaths. While the latest data from 2021-2022 doesn’t break out exact numbers for C. difficile, it does show a clear trend: as antibiotic use went up during the pandemic, so did hospital-acquired resistant infections-including C. difficile. That’s not a coincidence. Antibiotics are the #1 trigger. The worst part? Once you get C. difficile, treatment is brutal. You often need another round of antibiotics-sometimes stronger ones-and even then, it can come back. About 20% of people who get it once will get it again. And each recurrence makes the next one harder to treat. It’s a cycle that starts with a simple prescription for a cold or a sinus infection that didn’t need antibiotics in the first place.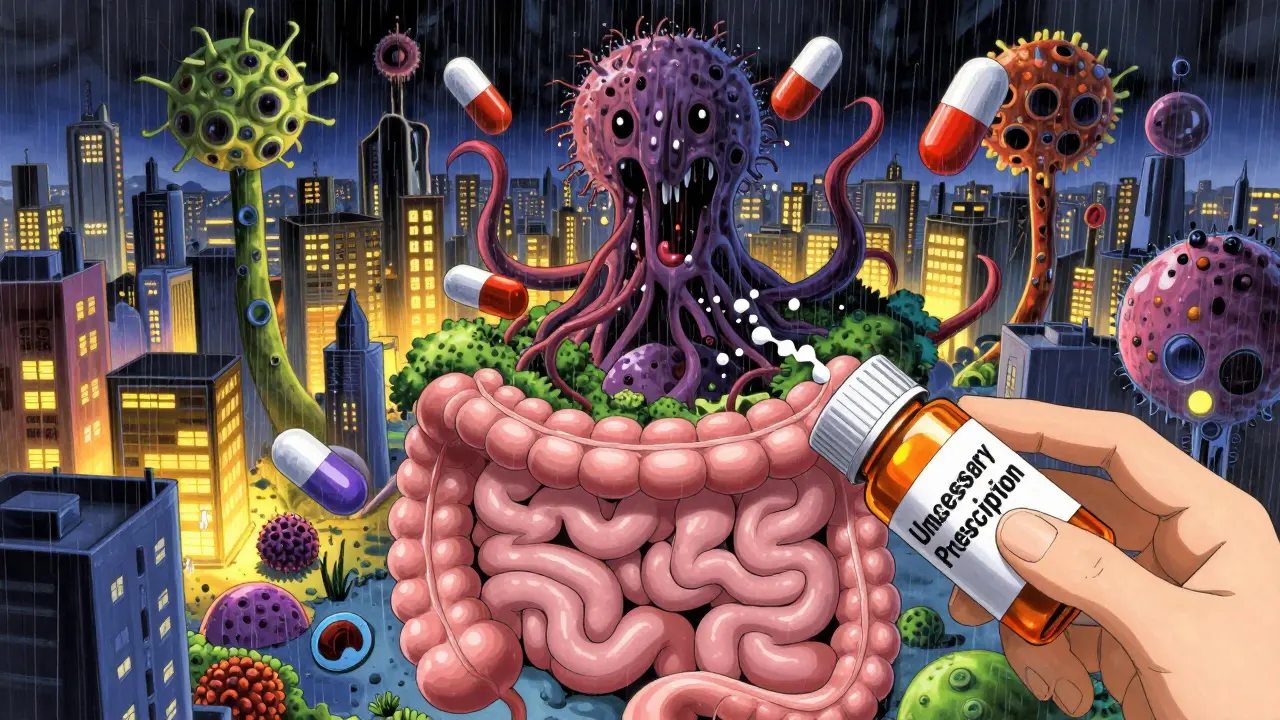
Why Doctors Still Prescribe Too Much
You might think doctors are careless. But most aren’t. They’re caught in a system that pushes them toward quick fixes. A patient walks in with a cough, fever, and sore throat. They want something to feel better. A rapid test for strep or flu might take hours. Antibiotics? They’re fast. Easy. And patients often leave happier when they get a prescription-even if it’s not needed. In low-resource settings, the problem is even worse. Without good diagnostic tools, doctors have no choice but to guess. If a patient has a fever, they give antibiotics. No test. No confirmation. Just hope. That’s how resistance spreads fastest-in places where labs are scarce and waiting isn’t an option. Even in wealthy countries, the pressure is real. A 2021 CDC study found that between 2012 and 2019, U.S. hospitals made real progress-cutting resistant infections by nearly 30%. But during the pandemic, all that progress vanished. Hospitals were overwhelmed. Antibiotic use surged. Infection control slipped. And resistant infections climbed back up.The Broken Drug Pipeline
You’d think with all this going wrong, pharmaceutical companies would be racing to make new antibiotics. But they’re not. Why? Because antibiotics don’t make money like other drugs. A pill for high blood pressure? You take it every day for life. A cancer drug? It costs tens of thousands. But an antibiotic? You take it for seven days. And when it works well, you don’t need it again. That’s great for patients. Terrible for profits. As a result, big drug companies have walked away. Since 2000, only two new classes of antibiotics have reached the market. The pipeline is empty. Organizations like CARB-X, a global partnership funded by governments and nonprofits, have poured over $480 million into antibiotic research since 2016. They’ve backed 118 projects. But even that isn’t enough. Only a handful of new drugs are close to approval-and none of them can fix the broad-spectrum resistance we’re seeing now. Meanwhile, 64% of countries report shortages of essential antibiotics. Some places can’t even get the basics. That means when resistance hits, there’s nothing left to try.
What You Can Do
You don’t need to be a doctor to fight antibiotic resistance. Here’s how you can help:- Never demand antibiotics for colds, flu, or most sore throats. These are usually viral. Antibiotics won’t help.
- Take antibiotics exactly as prescribed. Don’t skip doses. Don’t stop early-even if you feel better. Leaving bacteria alive lets them adapt.
- Never share antibiotics. A drug that worked for your friend might be the wrong one for you-or even dangerous.
- Ask your doctor: “Is this infection bacterial? Do I really need an antibiotic?” If they say yes, ask: “What’s the most targeted option?”
- Practice good hygiene. Wash your hands. Stay home when you’re sick. Vaccines (like the flu shot) reduce the need for antibiotics by preventing infections in the first place.
The Future Is in Our Hands
The numbers are terrifying. By 2050, antimicrobial resistance could kill 10 million people a year-more than cancer. It could cost the global economy $100 trillion. We’re not talking about a distant future. We’re talking about what’s already unfolding. The good news? We still have time to change course. Countries that have invested in antibiotic stewardship programs-like the Netherlands and Sweden-have kept resistance rates low. Hospitals that use rapid diagnostics and limit unnecessary prescriptions have seen C. difficile rates drop by half. It’s not about banning antibiotics. It’s about using them wisely. Every time you choose not to take one you don’t need, you’re protecting not just yourself, but everyone around you. Because resistance doesn’t care about borders, income, or age. It spreads silently. And once it’s here, it doesn’t go away. The next time you’re handed a prescription for antibiotics, pause. Ask the question. Make the choice. Your body, your family, and the future of medicine depend on it.Can I stop taking antibiotics if I feel better?
No. Stopping early leaves behind the strongest bacteria, which can multiply and become resistant. Always finish the full course, even if symptoms disappear. This is the single most important thing you can do to prevent resistance.
Are natural remedies a good alternative to antibiotics?
For viral infections like colds or flu, yes-rest, fluids, and over-the-counter symptom relief are safer and just as effective. But for confirmed bacterial infections like strep throat, urinary tract infections, or pneumonia, natural remedies won’t work. Delaying proper treatment can lead to serious complications. Always get a diagnosis before deciding.
Does eating meat raised with antibiotics contribute to resistance?
Yes. In agriculture, antibiotics are often used to promote growth or prevent disease in healthy animals. This creates resistant bacteria that can spread to humans through undercooked meat, contaminated water, or the environment. Choosing meat labeled "antibiotic-free" or from farms with strict animal health practices reduces this risk.
Can C. difficile be prevented?
The best way is to avoid unnecessary antibiotics. If you’re in the hospital, ask staff to wash their hands before touching you. Clean surfaces regularly, especially in shared rooms. If you’ve had C. difficile before, your doctor may recommend probiotics or fecal microbiota transplants to restore healthy gut bacteria after treatment.
Why aren’t more new antibiotics being developed?
Antibiotics aren’t profitable. Unlike drugs for chronic conditions, they’re meant to be taken briefly and only when needed. Pharmaceutical companies make far more money from medications people take for life. As a result, most big drug companies have stopped investing in new antibiotics. Public funding and global partnerships are now the main drivers of research.
Is antibiotic resistance a problem in my country?
Yes. Antibiotic resistance is a global crisis. While rates vary by region, no country is untouched. Even places with strong healthcare systems are seeing rising resistance in common infections like urinary tract infections and pneumonia. The WHO tracks resistance in over 100 countries-and all are reporting upward trends.

Chris & Kara Cutler
Just finished my antibiotic course for a sinus infection-turns out it was viral. I asked for a test. My doctor was impressed. Small win. 🙌
Rachel Liew
i had c diff after just one round of amoxicillin for a sore throat that was totally viral. it was the worst thing ever. took months to feel normal again. please dont take antibiotics unless you really need em. my body still hates me for it 😭
Jamie Allan Brown
It’s not just about individual choices-it’s systemic. Hospitals are underfunded, doctors are overworked, and patients expect a pill. We’ve built a machine that rewards overprescribing, and now we’re surprised when it breaks? The real failure isn’t the patient asking for antibiotics-it’s the system that lets them think it’s the right answer.
Nicki Aries
And don’t even get me started on the meat industry… I used to think "antibiotic-free" labels were just marketing. Then I read the WHO report on agricultural resistance. Now I only buy from local farms that show their animal health logs. It’s not easy, but if we want our kids to have functional antibiotics in 20 years, we have to vote with our wallets.
Deep Rank
Oh wow, so now we’re blaming patients for wanting to feel better? You know what’s worse than antibiotics? Being sick for weeks because your doctor won’t prescribe something because they’re scared of "resistance". I had a fever for 10 days once and they told me to drink tea. My cousin died from pneumonia because they waited too long to treat it. You think you’re saving the world but you’re just making people suffer. Maybe you should try living in a country where you can’t even get a basic test before they say "no antibiotics".
Ishmael brown
So antibiotics are bad? But what about when you actually need them? Like, I had a tooth infection last year and the ER gave me amoxicillin. If I didn’t take it, I could’ve lost my jaw. So now I’m supposed to feel guilty because I didn’t get a culture first? This post feels like guilt-tripping people who are just trying not to die.
Aditya Gupta
in india we dont even have access to good antibiotics sometimes. doctors give whatever is cheap and available. no tests. no follow up. resistance is growing fast here. but blaming patients? no. the system is broken. we need better labs, not more guilt.
Nancy Nino
Oh, so the solution is to just… ask your doctor? How quaint. I’m sure that’s why 70% of U.S. outpatient antibiotic prescriptions are unnecessary-because patients are just too polite to push back. /s
Donna Macaranas
My mom got C. diff after a routine hip surgery. She was fine for weeks, then boom-hospitalized for 3 weeks. It changed her life. I never ask for antibiotics anymore. I just say "what else can we try?" and it’s made a difference.
Lisa Rodriguez
Just want to add-probiotics aren’t a cure for C. diff but they help. I take them during and after every antibiotic course now. Not a magic fix but it’s one less thing to worry about. Also, hand sanitizer isn’t enough. Soap and water is the real MVP. Wash your hands like you’re about to perform surgery.
Nidhi Rajpara
Actually, I think the real issue is that people don't understand the difference between viral and bacterial infections. This is why education must start in schools. Children should learn about microbiomes and antibiotics in middle school. It's not complicated, it's biology.
vivian papadatu
My sister’s a nurse in a rural ER. Last month, she had a 14-year-old come in with strep. No rapid test available. The kid’s mom was crying, begging for antibiotics. She gave them amoxicillin-no choice. But she also gave them a printed sheet on antibiotic resistance, explained it in Hindi and English, and told them to come back if it didn’t improve in 48 hours. That’s stewardship. It’s not about saying no. It’s about saying: I see you, I care, and here’s how we do this right.
Doctors aren’t villains. They’re trapped in a broken system. And patients? We’re not the enemy either. We’re just scared. What we need isn’t shame. It’s access-to tests, to time, to education. The solution isn’t guilt. It’s grace, paired with infrastructure.
When I was in college, I got a UTI and demanded antibiotics. My doctor didn’t give them. She sent me for a urine test. It came back negative. I was furious. Two weeks later, I got sick again. This time, I asked for the test first. Turned out I had a kidney stone. Antibiotics would’ve masked it. I owe her my kidneys.
We don’t need more fear. We need more trust. Trust in science. Trust in doctors who take the time. Trust in our own bodies to heal when they can. And trust that the real hero isn’t the pill-it’s the pause.